Jen Schwartz is the founder and CEO of Motherhood Understood, a community for women affected by pregnancy and postpartum mental health issues. Jen had the perfect fairy tale vision of what life with a baby would look like. But, almost immediately after giving birth, everything felt different and she knew something was not right. She tells of how her mother described “the light going out of her eyes.” Today, she shares with us her journey through both postpartum depression and anxiety and how her recovery inspired her passion for helping to inform, support and heal the lives of other women who’s postpartum mental illness may otherwise have remained hidden in the dark. Motherhood Understood If you enjoyed this episode of the Down To Birth Show, please share with your pregnant and postpartum friends. Between episodes, connect with us on Instagram @DownToBirthShow to see behind-the-scenes production clips and join the conversation by responding to our questions and polls related to pregnancy, childbirth and early motherhood. You can reach us at Contact@DownToBirthShow.com or call (802) 438-3696 (802-GET-DOWN). We are always happy to hear from our listeners and appreciate questions for our monthly Q&A episodes. To join our monthly newsletter, text "downtobirth" to 22828. You can sign up for Cynthia's HypnoBirthing classes as well as online breastfeeding classes and weekly postpartum support groups run by Cynthia & Trisha at HypnoBirthing of Connecticut. Please remember we don’t provide medical advice, and to speak with your licensed medical provider related to all your healthcare matters. Thanks so much for joining in the conversation, and see you next week!
* * * * * * * * * *
Your coping mechanisms that you've had up to this point were great. They've gotten you this far. But none of these coping mechanisms that have made you good at life now work for having a baby. And so you're left like, you know completely naked and bear.
I'm Cynthia Overgard, owner of HypnoBirthing of Connecticut, childbirth advocate and postpartum support specialist. And I'm Trisha Ludwig, certified nurse midwife and international board certified lactation consultant. And this is the Down To Birth Podcast.
Childbirth is something we're made to do. But how do we have our safest and most satisfying experience in today's medical culture? Let's dispel the myths and get down to birth.
I'm Jen Schwartz and I am the founder of a platform and community called Motherhood Understood which is for women. If I couldn't buy a pregnancy and postpartum mental health illnesses that I founded after surviving postpartum depression and anxiety with my son. My son is seven years old now, when he was born, actually, when I was pregnant, I had this kind of fairytale vision of what motherhood was going to be like for me. I call it my I caught my Cinderella moment, I was going to magically transform into a mother but also a domestic goddess and a Pinterest queen and a breastfeeding champ. And I was going to take my baby everywhere and tell everybody how amazing motherhood was. And what happened instead was the day after I got home from the hospital. I started having thoughts of lying to get hurt so I could go back to the hospital and never have to take care of a baby and it was a huge red flag. I knew something was wrong. But I also didn't know what and I just thought that I was failing. And something was wrong with me that my whole vision didn't come to be a reality. And what happened in front of the fairy tale was I found myself in therapy appointments twice a week going on antidepressants for the first time. I'm quitting breastfeeding after five days because it was just it was making me insane. And I just couldn't, I couldn't keep up. Once the depression and anxiety were setting in, and I barely left the house, or even my bed for the first six months of my son's life, unless I was forced to a completely different experience. And nobody talked to me about mental health when I was pregnant. nobody talked to me about postpartum depression. I thought that it just meant I wanted to hurt myself or my baby. So when I didn't have those feelings, I didn't know that that was what was wrong with me. I also didn't think it was something that could happen to me either because I had a baby nurse lined up And I had family in town and a supportive husband. I didn't know that it was something that can happen to anyone. It really doesn't matter what supports you have in place or what your background is, and I didn't know what to do. And I didn't know where to go for help. And what happened was, I want to say it took me probably six weeks to really find the right help that started me on the path of getting better, which started off by going to my ob being prescribed anxiety medicine, and not she wouldn't diagnose me with anything because it was within the two weeks postpartum which could be baby blues. So she sent me home with a medicine for anxiety that stopped working after five days. I went to my regular doctor freaking out, he gave me something different. I made an appointment with a family therapist. And all she wanted to do is talk about ways I could be a good mother, which made me feel even worse because I didn't want to be a mom as you know at all. So girls on top of everything right? So much feel that I already felt like something was wrong with me. And then I just happened to after that Google postpartum depression, Charlotte, North Carolina therapists, and one woman popped up. And I mean, I called her I think it was a Sunday, he left her message and she called me right back and she fit me in the following day. And that was what started on started me on the treatment path to get better. I saw her once, sometimes twice a week between her and my regular doctor, we got me into a psychiatrist. I went on antidepressants. The first one we tried, it didn't work. So I had to wait another, you know, four, four weeks or so for the second one to see if it work and it did. But that was by then I was you know, at least two months postpartum. So I feel like a lot of time was wasted that I could have, you know, I can't get back now, but I could have had had I known exactly where to go for help and what was wrong with me. So I call it like a scavenger hunt. I like was on a scout. are one of those of sorts to find the right help and find information. And in addition to not having the information and you know, knowing what kind of professionals I needed to see to treat this, I also tried to find stories, you know, from other moms online. And it was really hard at the time. There were a few other ports. This is seven years ago, there were a few. But nothing really went past the surface. Nothing really shared those raw, intimate details. And I wanted to know that other people felt like I did, and I want to know when I was going to get better, and I couldn't find anything.
So Jen, we did a postpartum Roundtable. I think episode three and two of the women out of three confessed that they too had fantasies of being returned to the hospital so someone could take care of them. Can you share some of the really scary thoughts that you had? Yeah, of course, you know, you're the first person who's ever told me that they have friends. Other women say that they wanted to go back to the hospital. And as far as the thoughts I would have I didn't have intrusive thoughts where I, you know, could see things happening to my baby or worried that I was going to do something to my baby. They were more thoughts of making a mistake, I made a horrible mistake becoming a mom, why did I do this, I don't want to become a mother. I am failing at something I'm failing and everybody else on the planet is loving motherhood and doing such a good job. And there's clearly something wrong with me. And then there and then in addition to that, you know, maybe I would get in a little car accident and have to stay in the hospital for two weeks. And I didn't have to take care of my son and other people could take care of him for me and I could be taken care of at the hospital. So a lot of it was thinking that I made a mistake. And just feeling like I didn't want to be a mom and also really wanting to do anything to make me anxiety and those feelings go away. I would have done anything. Because it was it was so painful and the anxiety was so crippling that I couldn't do anything and I would have made I would have done anything to make it saw.
Jen, you were obviously willing to speak with your doctors and seeking out professional support and therapy. But how did you feel communicating these feelings that you were having to your husband, to your family, to your friends and what? What were their reactions? When
it came to talking to my husband and my family, I always say that I was lucky. I'm one of the lucky ones. My mom was staying with us at the time and she is a therapist. She now is treats postpartum women. But at the time she was she's a therapist a second career and the night that they actually got home from the hospital where I started having these thoughts and you could tell something was wrong. I promised myself I was going to say something to my mom that night. Not my Husband yet but my mom and I was about to and she cornered me and see she said john What's going on? So she actually ended up approaching me first and my husband had already said something to her too, that he felt like something was off. And a big thing for that was I didn't want to get out of bed so for him even though it was only two days in it was just wanting to sleep all the time, and not get out of bed. So I actually was lucky she said something to me first and then once she said that it gave me the space to tell her what was going on. But she'll also tell you like if you ever spoke to her that she physically witnessed the light go out behind my eyes like she saw the change. She saw it happened right in front of her.
There's a term that we use in the in the field where they say if a mom is checked out, like when the light goes out behind the eyes, that's a red flag and your mom and husband picked up on it.
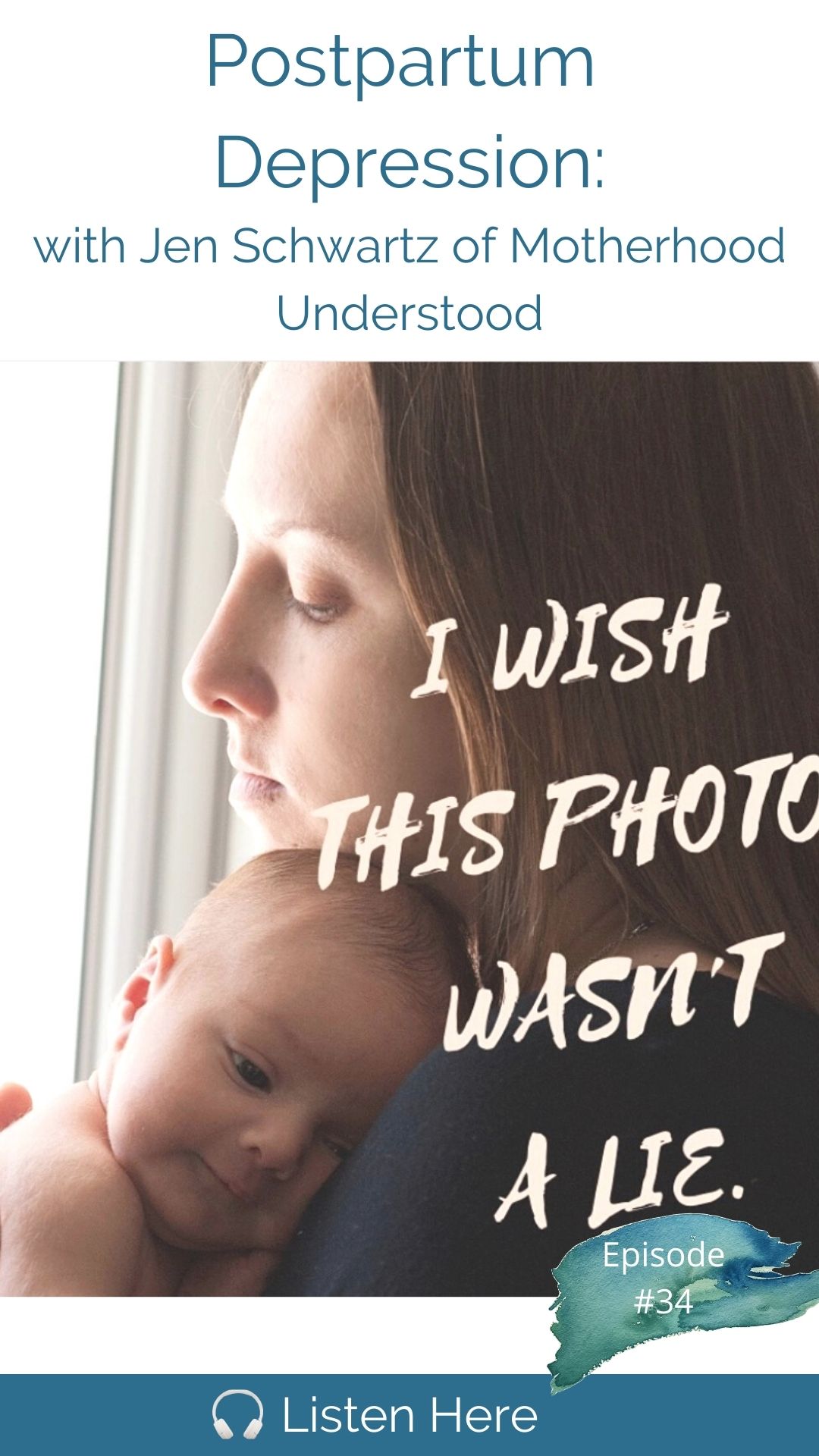
They picked up on it right away. So I was lucky and I always Joke once you're better, but with other women who have survived any mood disorder that if you lined photos of us up during the time that we were suffering, our eyes would all look the same, right? There's just, there's an there's a blankness behind it. My mom is the one that really helps me get on the path to getting help. She was the one that said, Okay, let's call the OB, she helped me find the right therapist, which then, you know, taught us that you have to see a therapist who specializes in pregnancy and postpartum mental health, it is a must that you find someone who specializes in it right. So that that for me was really helpful. And my sister was also staying with us at the time and she has suffered from depression and anxiety, through college and things like that. So she was very well versed in mental health, which was helpful for me because this was my first experience where I was diagnosed with something went on medication. I had seen a therapist before, and I had had, you know, panic attacks when I moved into my first apartment in Manhattan. And, you know, I could think of some times when I felt down in college and stuff, but never where it was like, Oh, I am depressed, I'm anxious, I'm taking medication. So my sister was really helpful with that. And my family actually was very supportive. I think for some people, it took them a little time to come around, or the more that they spoke to other people, they realize how common this was. So I was lucky. I was lucky in the in the family support department. So I started seeing a therapist and I remember the first appointment and she handed me a two sheets of paper. One was a scale, I don't know which scale it was, you know, to fill out to see how intense the depression and the feelings were. But the other was a sheet of risk factors for having a perinatal mood and anxiety disorder and I checked off a lot of them and I didn't even know risk factors were a thing. You know, if maybe they just want to even slip it into a folder when you're leaving the hospital or your birthing class. But what happened was, I didn't feel better, right? I was still the same amount. depressed and anxious. But what I learned in that appointment was it wasn't my fault. I had a lot of risk factors that set me up for that. Are you willing to share some of those risk scores?
But that would be I was given right I was given a diagnosis of postpartum depression. So now I understood what was happening to me. And I also learned that I wasn't alone. She told me she had treated thousands of women like me, and they all got better.
I think that's a really key point. To know that I will get through this like today is brutal. Tomorrow may be brutal, but I will definitely not live the rest of my life this way. Women have to have that bit of hope. And it is factual. So it's thank God we can say that to women that we do neuritis, it is temporary and it's nothing that you did to cause this.
Right? And so it gave a little bit of light, you know, to this darkness that I was in, even though and the thing is, is that when you're in it, you don't think you're getting better you think like I'm going to be like this forever. So even though every week I would sit on her bed couch, you know, hysterical crying but I would stay like this forever. She would promised me that I would get better. My mom would Promise me that I would get better and I didn't believe them, just because you feel like it's gonna be like this. So that cheat of risk factors, I feel like really changed everything. somewhere. How do you do you have a history of mental illness or a family history of mental illness? And yes, and also when I thought back to those times in my life where I clearly was depressed, or anxious, I just never did anything about it or put a name to it. So the answer is yes. I think one of the other things that was a big one and we don't talk about this a lot is are you kind of controlling a type a, you know, perfectionist personality, I was a teacher. You know, I like everything organized attention to detail. I like to be in control. High achievers, women at the high end of the socio-economic scale are likely just as women at the low end and we women are often harder muscles and use terms like control freaks, but really women who just are good at life. Exactly. Your house in order they have their career in order they take care of themselves there's food in their fridge they manage their lives well this knocks them exam that that doesn't make a woman a control freak, right? I mean, that's a whole other disorder. It's really a good thing. It's a good quality that it can turn against us because now we feel like a fraud. Like I'm not that woman writes her life in order at all right? Is that kind of what was happening?
Exactly. And so I, I was good at life. I was good at everything I got in early to college, I you know, I was good at life. And then I failed at motherhood and and what my therapist explained to me like this, and it was really helpful. She said, Jen, your coping mechanisms that you've had up to this point, were great, they've gotten you this far. But none of these coping mechanisms that have made you good at life now work for having a baby. And so you're left like you know, completely naked and bear and you have no idea what to do. And if you don't know about perinatal mood and anxiety disorders, You just think you're failing.
Yep. And there's one more you mentioned. And this one is really paradoxical. But it is also on the list of risk factors, women with expectations of being a wonderful mother. So I always think twice now, before I catch myself slipping and saying to a woman, you're going to be such a wonderful mother, because that's setting her up in all the wrong ways, right? It's like, we really want to lovingly lower their expectations of motherhood, and not say, oh, you're gonna be so great, because the moment they don't feel like they're so great at it, they think there's something wrong with them, or their baby would be better off without them. And you were that woman, people were telling you that you'd be wonderful and you expect it to be exemplary and a role model and good that too. And the paradox is that it sets us up for failure as much as having a history of anxiety or depression, which is incredible when you think about it, right? It's so true. And I also had, there were little risk factors to it I had, such as moving right before having a baby. We moved to our house three months before having a lot of family around at the birth and we're the first We're the first on both sides to have a baby. So my due date was actually the first night of Passover that year. And Passover is a big deal in my husband's family. So everybody came to Charlotte for Passover. So I no joke. I went into labor at the Seder table in front of 30 of my closest Jewish family members. And and, and then I also ended up laboring for 24 hours pushing for two and having a C section. At the time, I had thought I wanted and was supposed to do everything in my power to avoid a C section. Yeah, I just didn't know. And so Had I known that I actually would have really liked my C section. You know, I healed well, I was fine. I would have labored less, but I didn't know, if you'd had an earlier c section because our C section is a risk factor. But if you have a high satisfaction with it, it's it's arguably not one but if you had had a C section two hours into it, you might be you never know how you'd be hard on yourself. If you had done it that way.
100% Yeah, I think it's really about, it's about how we process whatever our birth experience was how satisfied we are right with it, whichever way it goes, right.
So all those things just, you know, set me up for this big bout of severe postpartum depression. Did you feel any of this coming on in late pregnancy? Did you have more anxious thoughts? Or was it really truly just like a switch overnight after the baby was born?
I really think what happened was that my expectations and it meet my reality. And it threw my identity into such a shock that my body went into shock and I physically got sick. And I remember sitting in my therapists office one time, I was complaining about the mom, I wasn't that I wanted to be. And she said, Jen, she said f those other moms, you're the mom you are and that's enough. And I still wasn't fully better at that point. But that really hit home for me, and I could just be who I am and that was good enough. Yeah. And that was wonderful, right? I think even if we do tell moms are going to be wonderful mothers, we have to redefine what what wonderful, doesn't mean every minute, right? I think we don't educate before the baby comes, we don't set up the supports before the baby funds, or even say to a pregnant woman, you might not love motherhood all the time, and that's okay. And they might not believe you, right? Because they don't know if it's their first time. But I think if we gave that space and provided that space, whether they listened or not it, it just opens up a new set of expectations that are Yes, lower, but awesome, more realistic. And I do do this now with people I know who are pregnant. You know, just kind of in a gentle, nice, friendly way, saying things that I wish someone said to me. I wish someone prepared me for a little bit.
Yeah, I think it's fair to say that being a wonderful mother, the one thing we could all probably agree on is simply responding to your baby's needs. And that's enough, right once the babies needs are met, even if that mother is experiencing anger or depression or weakness, she's picking up that baby changing the baby. And I think that's where we should set the bar. Like if the question is, is this baby getting responded to or the needs being met? If the answer is yes, now what can we do for the mom? Let's surround the mom and get on what she needs. Let me ask you this before you continue with your story, can you name the emotions that you're feeling on a regular basis in the spirit of your life? What were the emotions you kept feeling? on daily basis?
There was a lot of grief and regret. You know, grief, I think for the way things were before, you know, regret for you know, ruining my life per se. The anxiety was the most prevalent so even though I was diagnosed with postpartum depression, the anxiety was the worst of it. I was how did that manifest itself? What did that look like for you?
For me, it's weird. So for me But anxiety kind of went with the depression because like I said, I couldn't get out of bed. And I didn't want to, but I would still lay there feeling like there was an elephant sitting on my chest, and my heart would my heart would race. And even if I fell asleep at night, I woke up every morning at 3am like clockwork, I just woke up and I couldn't go back to sleep. And it was just this awful racing heart lump in my throat, feeling that I couldn't get I couldn't get rid of. And if I did get out of bed, I would walk I would go outside and I would walk circles around the cul de sac in my neighborhood, because my mom told me that movement could help a little bit and I think maybe it said, I'm not, you know, but I would, I would walk every day I could get myself out of bed crying on the phones or for that I would never get better. Like I was probably the crazy lady in my neighborhood, you know, like walking in pajamas. And I had one friend, an older mom from whose kids were older and she had actually came over almost every day and sat with me. And she would get me out of bed. And she would make me go for it. She would take me for a walk. I never knew people walked in the mall until I had quit from depression. So if it was raining, we would drive to the mall. And she would we would walk the mall until the anxiety kind of came back and I would say I have to go home and she would drive me home. I remember there was one day, there was a break between when we were going to have someone help us during the day. And her mom came over and watched my son. And she took me for a walk. And then my friend she put me back in balance she wrote and she rubs lotion on my feet until I fall asleep. And I remember thinking like, I haven't shaved my legs and we like it but it didn't matter to her. And then this one friend also she would keep everybody else updated because it was also I was tired, right I was exhausted. This really takes everything out of you. So I didn't have the energy to socialize. lies are really, you know, text back a friend or call back a friend. So she would send emails and texts and kind of keep my other friends in the loop about what was going on. And so it's almost like I had a point person, I didn't really have to worry about providing updates or explanations myself, which was really helpful.
Imagine what women do when they don't have the support you had so much. Right.
Right. I had so much support. And I think, you know, looking back on it, I just right. I was lucky, I was lucky to have the family that I have to have the resources and the access to getting into therapy and getting medication right away and also having my husband and I had, you know, he was really supportive. He came with me to a therapist appointment, you know, so he couldn't really kind of learn more from her what I was going through and what we needed from him, which I recommend, you know, everybody brings their partner to a therapist appointment i get i get the question a lot. How did you get your partner to understand And I mean that's a whole other conversation how you know we really beat needs to be included partners in this whole conversation and in the education piece.
Down to Birth is sponsored by Postpartum Soothe. Recovering from a vaginal birth takes many women by surprise. Everyday activities like sitting, walking and going to the bathroom can be uncomfortable, and Postpartum Soothe is just the remedy to support your healing and relieve discomfort. Postpartum Soothe is a 100% organic herbal blend that's applied to maternity pads in the days immediately following your birth, giving you all the benefits of a sitz bath 24/7. That's because herbs like comfrey leaf, uva ursi and witch hazel are known for their antimicrobial and anti-inflammatory properties. Postpartum Soothe can be prepared at any time during the third trimester and it makes a beautiful baby gift. It's a must for any woman seeking a faster, easier recovery from a vaginal birth. Visit postpartumsoothe.com and use promo code DOWNTOBIRTH.
So other emotions I felt were a tremendous amount of guilt and even shame that I, it was like I became a mom and I needed medication. Right there was there was a level of shame and guilt to that initially when that happened, and exhaustion was a huge one. I think that that's just part of the, you know, part of the depression and the sadness piece. But exhaustion was huge. I really had no energy to do anything but sleep and just lay there. And the guilt was big too. I remember binge watching during postpartum depression, The Good Wife all five seasons, and I remember laying in my bed thinking, wow, like this is this the guilt I should be taking care of my baby but I'm laying here binge watching The Good Wife because I can't bring myself to anything else. So there was a lot of there was a lot of guilt for sure. And I think at first to a little embarrassment, you know that hesitation of what are other people that are, you know, friends or people who knew I was pregnant and so excited to be a mom, what are they going to think of me? Right? What are they going to think about the fact that I again became a mother and ended up in therapy and on anti depression. So for me, at six months, I started to see some light I started to feel better. And I had all these I describe it by having all these firsts I had all these firsts. So then I had been on my antidepressant combo and anxiety medicines that have you know, been working since I guess they've been working for a few months now. I you know, still in weekly therapy. And but I had first so I gave my son a bath before my husband came home from work. I volunteered to do it. My sister was staying with us and we gave him a bath. never done that before. I have six months, put my son in the stroller and walk to the park. Just the two of us never done that before. I went to my first hot yoga class, which was something I did a lot before I was pregnant. And I went on a date night with my husband, and we went to a concert and I had fun, and I wasn't faking it. And the smile wasn't fake. And slowly, I just would have more good days, the first turned into seconds and thirds, I would have more good days until I didn't even realize anymore that most days were good. And it wasn't a year I remember. It was in a year at my son's first birthday. I you know, and I remember looking around and it was at my father in law's house. And I mean, there were a ton of people there. We had a catered friend's family. And I remember just looking around at everybody, and these were people who, like stood by, you know, they stood by me and they stuck with me and they knew what I went through. And there was so much love in the house and I finally felt on that day. It was like, yeah, I'm a mom. I can do this. I love my son. I'm as confident as I can be. I bought this. So it was really at that full year. I still get chills when I, you know, think about that or talk about that. But that was when I started to feel better.
Chen When was the first time you realized you were intensely bonded to your son? You were just like madly in love with him. couldn't get enough of him. How long did that take?
It was it was sometime between the five and six months. I think it was the six months and I think it was another first so I have another really good friend, Renee, she was my very first friend to have babies and I used to cry to her during postpartum depression. She had two boys. And I would say I love your boys. I've always loved your boys. Why don't I love my like, why don't I feel close to mine? And we were at their house. I think Mason was about six months and I was throwing or throwing him up in the air and catching him and cooling on him and loving on them. And I think that was the moment and she actually sent an email behind my back to everybody that just goes she's back.
I think it's so important for women to hear that message because it's such a fear for Women who experience postpartum depression and anxiety that they will never recover this missed opportunity to bond with their baby if they if it doesn't happen in those first days. I mean, we've even had women say that they're worried that if they miss the golden hour with their baby, that bonding will never happen. And here you are saying it was six full months before you had your real first feeling of connection with your baby and right and your bond with your son is no less than anyone else's.
It's true. And I think that it's another expectation that if we could set before the baby comes and prepare women that it's not what's the Pampers slogan, love it first touch for everybody. You know, those things mess us up, they really get in our heads and they mess up. And it's really common for it to take time and to get to know each other. It's not always a natural thing. And it takes time and it's okay and and also to I also think I realized too at the I'm not really an infant person, even, you know, even with friends, babies, I'll hold them. They're cute. I give them back. So it's also okay to not love the infant stage and love the toddler. So true. It really is such a different experience for each each woman.
What were your stages of getting better and I'm sure a lot of people listening would also love to know how, if and how you ever weaned off of those meds.
So, my stages of getting better. Honestly, were just sticking to my treatment plan and having faith and patience, which is so hard when you feel like you're in this hell that you're never going to get out of it was the therapist appointment once or twice a week, taking my medication, you know, and being open minded about the medication, going for those walks and being sad and you know, not pushing anything down or ignoring anything. But I think the key really is the sticking to the treatment of the combination of the therapy and the medication. And I actually I'm still on my antidepressants. When I first started writing before I launched motherhood understood my blog was called the medicated mommy. I have a jean jacket that says the medicated Mommy, I think there's no shame in taking antidepressants. And I think they really, they're really helpful. And I think for me, what it allowed me to do was get back to my baseline where I had the will to go to the therapist appointment and talk about my feelings and the will to fight. I also this is gonna sound really weird and silly, but there was a song from a TV show that was on during the time I think it was called Smash. It was like a Broadway musical type TV show. And there was a song in it and I don't even remember but when I started to feel really, really anxious, I would repeat the chorus to myself in my head over and over again and it would actually calmed me down. So having something like this, I think now there are so many wonderful apps To help, you know, with meditation and calming things that we didn't, I didn't have back then. But I think those practices were really good too. I try to be open and talk about my feelings as much as I could with with my husband. And having that one friend, right, having that one friend who came over and then updated everybody else, I highly recommend if you have like your one, you know, you're one person that you can really fall apart in front of that maybe isn't your you know, that maybe isn't your partner that was really helped. That was really helpful too. And then once I got better, and started to have good days, and feel like I could take on more, the yoga how the yoga started to help, but that was six months in.
It's always impressive to see people who can take their pain and their challenge and turn it into such a passion like you have and reach so many people. Yeah, thank you.
How did that come about? What was the first stage for you when you felt like you could look outside? yourself and provide something to other women.
So I basically, I decided when he was two and a half, I was going to start a blog just to share my story. So I launched a blog on January 1 2016. And I called it the medicated mommy. And all I did was share my story. And I wrote those raw intimate details about my feelings how I knew something was wrong. The treatment I found to get better and all about the medication I took, you know, everything you need them and I wasn't I just I was an open book. I there was nothing I wouldn't share. And what happens was, I would get messages and, and comments from so many women saying Me too, and I realized the power of story sharing. And then, three months after I lost my blog, I went on a women's retreat, fall camp power men. And I didn't know what I was getting myself into. I signed up I went across the country to California for this women's retreat completely by myself. By the end of the weekend, I had all these women who I didn't know before telling me how much they loved my honesty and my confidence and my bravery and my voice and how lucky Mason was to have me as his mother. And I was like me that medicated Mommy, you know, I mean, those were not things that I had ever heard of. When I bought home. I wrote an article for my blog. And I posted it. And I sent it to the founder, and she just suggested you should send this to Arianna Huffington. And Huffington Post, it was when she's still around, I have posts. And so I did. And she wrote me back within 24 hours, and I became a contributor on Huffington Post. And that kind of that was what started me writing for other places. So I would start writing and I wouldn't be published I'm scary mommy and have quotes in cafe mom. And eventually I just didn't want this to be about me anymore. And so I transformed it and so what you've seen today as motherhood understood which you To me is about all the mamas right? All the one in five women who are affected by these illnesses every year. And it's become a platform and a community and a story sharing hub for these women, where we are committed to providing community and support and education and resources. So no woman has to go through this alone or ashamed like I did. And every woman gets the treatment that they need to feel well for these illnesses that are temporary, so they can enjoy motherhood. So that was really the power of story sharing. I think that led me here because I think that the story sharing is what is going to ultimately be the most effective cure for the stigma and the shame that still surrounds maternal mental health. The one thing that really really got me was I posted the picture a year ago, I post that and on Instagram and it was a little kind of micro blog, but the picture said I I tried To give my son a happy, healthy mommy instead of a sibling. And it was my very first post and everyone viral, it was picked up by a few publications. I think there were over, you know, hundreds and hundreds of comments of people who resonated with that. Really, I never expected that. That really made me feel more seen than anything ever. I didn't know that there were so many women out there like me who just decided that having one child was the right decision for their family, a large part as a result of having a perinatal mood and anxiety disorder, but also for other reasons. A lot of women think that they get past let's say, the six week mark, and they're in the clear, right? Because for me, mine happened so quickly, right? The day after I got home from the hospital, which, you know, they they tell you to look out for baby blues, but we knew that mine wasn't that it was just so intense. The feelings were so intense, but you know, we have women who are 12 months postpartum, I don't think I realized when there's started. And part of it was because we use postpartum depression as the term for everything. And now they believe we use Perry needle, that it really is for, you know, Pregnancy through one year. But there are plenty of women who will go into a therapist two years postpartum. And have these feelings of postpartum depression or anxiety or OCD or whatever it is, because they never got resolved earlier. Yeah,
I think what's surprising is when they coast for a while for six or nine months, and then it suddenly strikes them so to speak. I think if there's one thing I wish I could change, about the lack of knowledge around this field, if I had to pick one thing, it would be that this is not a hormonal issue, because I think that leads women into believing if it's going to happen, it'll happen early on, right in that fourth trimester. It certainly leaves no room for support of partners, no room whatsoever. It's your adoptive parents. And I think that's the thing and i and i personally, I don't know why This is just me, this has always been me. I have always rejected chalking off anyone's emotions as being linked to hormones. I'm not into women calling themselves hormonal, or anyone accusing a woman of being hormonal or even accusing a two year old of just acting like a two year old. Right? Our feelings are legitimate, but by the misinformation that this is hormonal, is where is the root of a lot of the lack of support that we see in our nation?
Yeah, I think so too. And I think also the other thing because you brought up you know, adoptive parents, which you can empower all of this adopting a child is also the amount of women who have gone through a miscarriage and infertility, treatment and you know, any type of loss who have their baby and think that everything is going to be magical and wonderful because they wanted this baby and they wanted to be a mother for so long. And they get hit with these feelings of regret and depression and anxiety and they have no idea what's going on because they their mental health was not discussed with them. And that is something that over this time has really gotten to me. Because in itself in fertility, treatment and miscarriage affect your mental health, and they are risk factors. And that is a an area that I don't be we're providing enough education. I just, it's horrible.
Yeah, there's a host of risk factors that are linked specifically to extraordinarily high expectations of what motherhood will be like. So like that of being a wonderful mother, older moms, moms who do IVF their medications gets so high that it's, you know, the reality compared to the expectation is there's just a bigger discrepancy, right and be just a harder blow.
Right. And I just wish, you know, you know, for a mom who's going through IVF that she know, I reappointment you know, even a mom who's just going for her who's pregnant and going through her regular or, you know, ob visits, you know that you see a counselor or something and they tell you, you know, look, your mental health is at risk due to these IBS treatments. And, you know, here's education, it's really having almost being given a postpartum mental health plan, in a sense, we are going to be launching a one on one postpartum mental health planning service, that we're going to be offering women and their partners before the, you know, to set up an entire plan that they have for when the baby comes in the event of a mental health issue. Every number is listed. They know who the local you know, specialists in their area are they have a code word you know, that they use with their husbands or, you know, partners, when they need to tap out, you know, they have, what they're going to be responsible for and what they're going to delegate out you know, all things that we don't really think about. Before the baby comes, I just wish all women and their partners knew that perinatal mood and anxiety disorders are common. And if you are suffering from one you are not alone and you will get better even when you're in it and you feel like you're never going to see the light, there is light and it is worth fighting for to get to the other side.
If you enjoy our podcast please take a moment to leave us a review on Apple podcasts and share a favorite episode or two. You can follow us on Instagram and Twitter @downtobirthshow or contact us and review show notes at downtobirthshow.com. Please remember this information is made available to you for educational and informational purposes only. It is in no way a substitute for medical advice. For our full disclaimer visit downtobirthshow.com/disclaimer. Thanks for tuning in, and as always, hear everyone and listen to yourself.
Recent Episodes
Subscribe
Between episodes, connect with us on Instagram @DownToBirthShow to see behind-the-scenes production clips and join the conversation by responding to our questions and polls related to pregnancy, childbirth and early motherhood.
You can reach us at Contact@DownToBirthShow.com or call (802) 438-3696 (802-GET-DOWN).
To join our monthly newsletter, text “downtobirth” to 22828.
We'd love to hear your story.
Please fill out the form if you are interested in being on the show.
Subscribe to The Show
Follow Us On Social