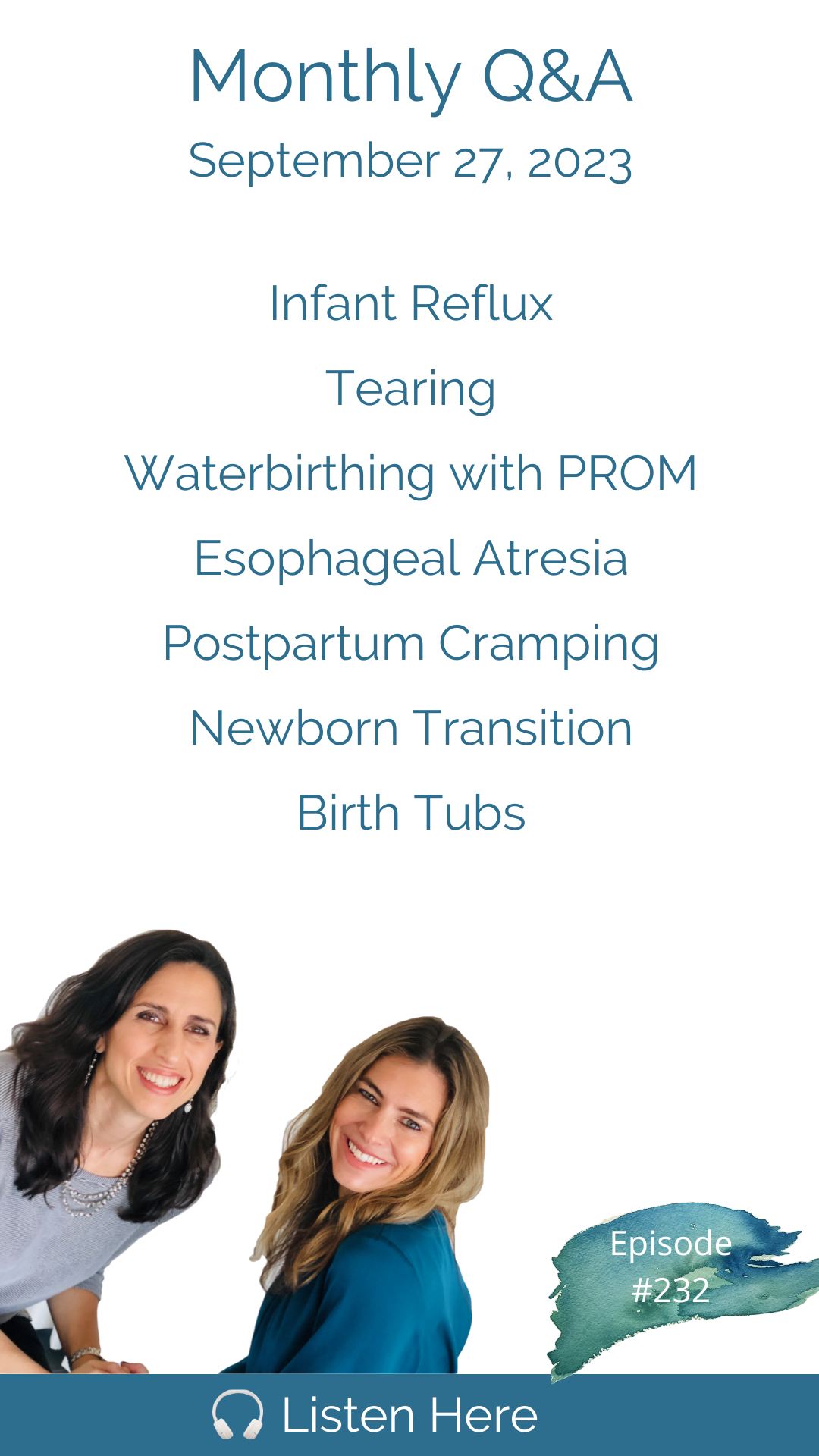
Hello Friends! It is time for the September Q&A episode! Today, we open with two listener emails sharing their experiences on declining circumcision and accepting a necessary emergency cesarean birth. Next, we dive into your questions beginning with: Can I still labor and birth in the tub even if my membranes have ruptured before labor begins? Lucky for ya'll, we have Barbara Harper of Waterbirth International pop on the show to answer this question. Next up, we address whether experiencing a 3rd or 4th-degree tear during your first birth should deter you from pursuing a subsequent vaginal birth. Does it categorize you as high risk? We'll explore this important topic. Seeking more comprehensive solutions for infant reflux beyond the basics? We've got you covered. Then, we tackle the dilemma of giving birth at home when it feels safest, despite not feeling the most relaxed due to working from home. We'll share valuable perspectives on making the right choice for you. Curious about the accuracy of ultrasounds in diagnosing esophageal atresia? Liz Eidelman, a mother of a baby born with EA, joins us to answer this question. And that's just the tip of the iceberg! In our extended version of this episode, available exclusively on Patreon and Apple subscriptions (ad-free, of course), we delve into a treasure trove of topics, including ABO incompatibility and jaundice, alternatives to ibuprofen for postpartum cramping, the newborn transition, nuchal cords at birth, and much more! As always, we close with quickies and a personal question about the best advice each of us has ever received. PS: Don't miss the outtake at the end of every episode. Connect with us on Patreon for our exclusive content. Work with Cynthia: Work with Trisha: Please remember we don’t provide medical advice. Speak to your licensed medical provider for all your healthcare matters.
**********
Down to Birth is sponsored by:
Needed -- Optimal nutritional products for before, during and after pregnancy
Modern Nursery--Your one-stop shop for eco-friendly, stylish baby gear
DrinkLMNT -- Purchase LMNT today and receive a free sample kit.
Love Majka Products -- Support your milk supply.
Silverette Nursing Cups -- Soothe and heal sore nipples with 925 silver nursing cups.
Postpartum Soothe -- Herbs and padsicles to heal and comfort.
Email Contact@DownToBirthShow.com
Instagram @downtobirthshow
Call us at 802-GET-DOWN
203-952-7299
HypnoBirthingCT.com
734-649-6294
Hi ladies, my name is Hannah and I have a question about ultrasound accuracy. I was holding my 20 week scan that baby looks completely normal and on track but they did not see a stomach feeling which would suggest that his esophagus is not connected to his stomach, which would be known as esophageal atresia, or tracheal esophageal fistula versus about premature rupture of membranes and water birthing, I know that there's no increase in risk of infection, just one of the things straight up. There's even a line in iron amaze guide to childbirth where she kind of put some parentheses, you know, labor in the tub, unless your membranes have ruptured. And they for mice son, was told by the pediatrician that we needed to get into the NICU due to the extreme jaundice,
be like a giraffe, like a giraffe, everyone likes a lot easier from from that place. And don't always pick up the check for everyone.
You can't do that we still have to have some kind of balance of practicality in life.
I'm Cynthia Overgard, owner of HypnoBirthing of Connecticut, childbirth advocate and postpartum support specialist. And I'm Trisha Ludwig, certified nurse midwife and international board certified lactation consultant. And this is the Down To Birth Podcast. Childbirth is something we're made to do. But how do we have our safest and most satisfying experience in today's medical culture? Let's dispel the myths and get down to birth.
Hello,
it's been a while
my microphone had dust on it.
It hasn't been that long. Welcome to the September q&a episode. It feels like it's been a long time.
It feels like it's been a long time because we're usually here every week. And it's been a few weeks.
You had some other work to take care of that was fun on the side. And you got to go up to Cam. And that was good for you.
Yeah, it's a little hard to record from Canada. Yeah,
we don't we don't even try.
But here we are. And we are happy to be back. And we have some really fantastic questions today. As always, yeah, you guys submit amazing questions, and we love answering them. But before we begin, do we have anything that we want to talk about?
I wanted to share an email that we got actually we got two that were kind of cute and interesting. Well, the first one is from a listener, whose name is Anna. And she wrote Dear lovely ladies, I just wanted to express how much I love your show. I started listening as soon as I found out I was pregnant. Being educated made a huge difference in my birth and gave me the confidence to ask questions and advocate for what I wanted. I had my daughter back in March and wanted to share a bit of my experience. My birth didn't go as planned. But because I was educated and I had a care team that I trusted it was much easier to process the experience. I had with someone say many complications in my pregnancy, gestational diabetes and insulin GBS thyroid issues, SPD symphysis pubis discomfort and being 32 with my first pregnancy. Wait a minute. Why?
See she thinks she's old. What?
Being 32 Someone convinced wraps that off the list. That is such a shame that anyone would believe that. All right, my my first midwife was not what I expected. Maybe she's the one who convinced her being 32 for the first pregnancy is not sufficiently young. My first midwife was not what I expected. So I had the courage to find a different midwife and team that was the best decision I made. I didn't want to be induced. So I was very thankful that my daughter decided to come at 39 weeks, and that was convenient. Everything with my labor started perfectly and was manageable. But unfortunately, I got stuck in transition for several hours and fetal monitoring revealed she was in distress. At one point she even started to go back up. Despite my walking and using the peanut ball. I ended up with an emergency C section and it was handled in the best way. I didn't feel pushed into this into the decision. And my midwife and nurses did everything they could to calm my fears. It turned out that my daughter had the cord around her neck several times and was so tangled that you couldn't descend. Hence why I was stuck in transition for so long. Even with all the medical intervention I ended up having I still had a beautiful peaceful birth. My daughter took to breastfeeding like she was born to do it, which she wants, which she was yes. Thank you again for doing the work you do to educate and encourage women to advocate for their care attaches a photo of myself and my sweet baby Amelia. Much love. Yeah, and she attached her beautiful photo. So I wanted to share this. Because, you know, we know we get birth stories all the time. But what's important about this one is that I think that sometimes when women are pregnant and they're working so hard and planning, they're under the misconception that this whole thing is riding on whether they have a vaginal birth or a C Section. But when women are really prepared, and they do invest the time and knowledge into their birth plan, they really can end up with a more satisfying C section should it go that way. And so often women are saying, Thank God I was prepared. And I because my C section would not have gone as well as it did. So when you have a C section, yes, like she, this woman said it perfectly, she was a part of that decision. She was treated with respect and care and involved in everything herself. And you focus on the same breathing, keeping your physiologic physiology relaxed, and then you focus on bonding. I mean, really, there's so much of the process that is involved, that mirrors a vaginal birth, it's just the baby emerging comes differently. But I just appreciated this message, because I want women to know that it is never a matter of just throwing it all away. It always serves you to be prepared and educated no matter how your birth evolves.
And also, I think it's important to just acknowledge that when you feel that the C section is necessary, it's so much easier to accept. And when we're talking on the podcast and on Instagram about the excessive use of interventions in maternity care, we are always referring to those on the necessary Syrians, which are so many to many, but some are very necessary and needed. And we're very grateful and appreciative that we have that. It's just figuring out that gray area of when a when a C section is actually needed and when it's really just done because it's a little bit more convenient.
Right then when you're really well prepared and informed you end up actually grateful for the C section because if you're not feeling grateful, then you don't believe you need it and you would decline. Right. That's what comes with the education as well. But anyway, really beautiful story. I was so happy to receive that on our behalf.
Yeah, and thank you to our listeners for sharing we always are really excited to see the follow up with your birth stories and especially when they come a little photo of the baby. Alright, this was a cute little story from a woman named Karolina and she is Polish. She's been here a long time she's fluent in English, but her sister is not fluent in English whatsoever. And this according to her story, and this is what she shared. She said hello, Cynthia and Trisha, I would like to share a silly little story with you. My sister came to the US from Poland when she was five months pregnant. It was very important to her that her son not be circumcised at the hospital after birth. She didn't speak English. So she asked a friend of ours that was fluent, how to say do not circumcise in English. For months leading up to the birth she repeated the sentence over and over and had written it down so that she could advocate for her son once he was born. My sister, her husband, and sons moved back to Poland when the new baby was three months old. They've lived there ever since. And understandably, she does not have to speak English there at all. I've recently become very interested in birth and doing lots of research, including listening to your podcast, and decided to ask my sister about her births and what those experiences were like for her. When she was telling me about her birth story. She recalled that she had to learn how to say do not circumcised in English. And she said let me see if I can remember how to say it. And then she said do not circumcise. I have lived in the US since I was 14. I'm fluent in English, so she wanted me to let her know if she remembered it correctly. I was stunned. She said it perfectly. The reason I was so surprised was because her son is now 19 her mama bear brain recognize that as so important that to this day she knows how to say it. I can't wait to become a mother as well and experienced that level of protectiveness. Thanks for all that you do Carolina
what I love about that is that it was just three simple words. Do not circumcise, it wasn't some long drawn out explanation or question or you know plea. It was simply do not circumcised full complete sentences. All you have to say
that's true. Yeah. Okay, but those were worth sharing. I hope so. Definitely. Yeah, definitely. Alright, so
shall we dive into our questions?
Yes. And I'm so excited about the first one because once again, Barbara Harper has come through for us and answered the question about water birthing. So here it is.
Hello, this is Jessica from Atlanta. Love your show. Calm. I got a question about water birthing. I definitely would love to do that. I'm super early in pregnancy right now. But my question is about premature rupture of membranes and water birthing. I know that there's no increase in risk of infection. Just one of the things straight up. There's even a line in iron amaze guide to childbirth book about water birthing where she kind of puts in parentheses, you know, labor in the tub. Unless your membranes have ruptured. Maybe I'm interpreting that wrong or but I guess I'm just curious, you know, let's say your water breaks pretty early, and you're starting to go into active labor as well, 24 hours later, or whatever it may be. It's still safe to labor and birth in the tub with your membranes ruptured. Thanks so much for all you do, I can't thank you enough. I owe you listeners of down to birth podcast. This is Barbara Harper, founder and director of Waterbirth International. And today I'm going to talk about ruptured or released membranes. And when you can get into the water, we have a question from someone after she read Ina May Gaskin's Guide to Childbirth, that it was not recommended that you should get into and labor in water with released membranes. I want to correct that you can labor and water anytime, after your membranes have released, even if you're not in labor, I take women's swimming, I recommend I do flotation sessions with them in early labor. And often using the water for deep relaxation and comfort. It changes your brain chemistry. And you'll start releasing more oxytocin, the more comfortable you are. So it often is a good way to begin the labor by taking a bath or being in the swimming pool. And nothing has been reported in the literature that say says that there's an increase in infection rates. I think that was when I may published her book. Originally in 2003, there was an update in 2008, there still was a discussion on whether or not the mother or the baby would get an infection. And it just hasn't proven. I want to show you or tell you about a study that was done all the way back in July of 1996. And I remember having a discussion at a midwifery conference with the authors of this study. It was Margaret Erickson, Lars Ladd force and Lars Matson in Scandinavia. And what this article did was they did a randomized study of 1385 healthy women. And during the first stage of labor, 538, women decided that they wanted to take a bath 847 did not all of them had a pre labor release of their membranes. And some of the women waited up to even 72 hours after those membranes have had released before Labor began. None of the women had any digital examinations of the cervix until they were in active labor, which meant six or seven centimeters. And the results of that was that 1.1% of the bath group had a mild Cortijo amny Unitus, which was treated with antibiotics. Some of the babies were affected, but there wasn't any difference between the groups. So the conclusion, even back in 1996, was that a tub bath did not increase the risk of maternal or neonatal infection after premature rupture of the membranes, even with a long latency or a period of time before Labor began. So I wanted to clear that up and reassure you all that you can use the bath at any time with intact membranes and without intact membranes. So I wish you well, good births for everyone. And if you have any questions about waterbirth just drop me a note. And also if anyone would like a free one hour video that I've recorded on waterbirth I'm happy to send it out. Just go on to waterbirth.org or send me an Instagram message at the Barbara Harper on IG or my email address is barbara@waterbirth.org. So take care, God bless. Bye bye.
Thank you, Barbara, as always for being there for us and our listeners. right on to the next.
Hi my name is Shelby. I I spoke to a few ladies who had terrible tearing at their births. And they are really afraid of home birth, they're really afraid of hospital free birth without intervention, because they're just so scared, they're going to tear again, some of them are considering C section. And I just find that really sad. Is there any evidence that tiering automatically puts you in a high risk category? And then to like third or fourth degree tears, not just, you know, first or second? Anyway, I really interested to hear your thoughts on this. And thank you for your show.
I would never say that you should not attempt a vaginal birth because you had a third or fourth degree tear the first time and doctors do tell women this. I wouldn't agree with that. Because the perineum heals fully. And how you give birth the next time around just just doesn't mean you're going to tear again, if you tore like that the first time. There's so many things that go into whether or not you have a tears and many things that we can control.
So many things diet, position of the baby position of the mother. There's an horse of pushing, you know, I had I remember my first client who had a fourth through the tear. And you can imagine the anxiety she had having her second baby she was so scared. No one suggested a C section. She had his her second baby and she didn't tear at all. She did go to a pelvic floor specialist and learn a few things. Apparently she had a weak pelvic floor now everyone listening is going to be afraid they have a weak pelvic floor. She had a weak pelvic floor I think unusually weak. Apparently she was tearing long before the baby even fully descended. The doula had explained that but she didn't tear it all with some work and preparation but I feel like this is a new trend because this week we got three or four questions about this Trisha doctors saying well, you should have a C section next they're just looking for the next thing now they're acting like tearing is worse than a C section is not a third or fourth degree tear. Ina may Gaskin statistics were point 4% for women per 1000 had a third or fourth degree tear a per 1000. It's really rare. But going to C section that's a that's a big deal.
And we can't underestimate nutrition in skin integrity. So it is really important that you do have good healthy nutrition, adequate nutrients, vitamins and protein in pregnancy because it does that can impact we do it is more common for women who are really nutritionally deplete like really depleted to tear more.
Nancy Waner always says it's um, minerals, especially it makes sure you have high mineral diet is your element.
Hi, ladies, I have a question about reflux. At about four or five weeks, my little guy developed some reflux symptoms, he didn't want to be late button his back, he was putting up a little bit more, you could almost like hear and see the reflux when you would after he would feed and he would try to lay him down. And so I'm just curious if you have any suggestions besides the obvious ones that they always give you up right after you feed you can elevate elevate their head when they're sleeping or laying down. Trying I've been told by one source to speak feeds out longer and another source disease closer together. But I just feel like all of the answers I'm getting are just treating the symptoms of the reflux, but they're not addressing the root cause of why it's happening. And so I understand there are some, you know, immaturity is in the infant digestive tract. And that certainly plays a role in reflux. But in the you know, intuition tells me that there's another root cause to why it's happening. And I've just not been able to figure it out. And I've not been able to find any information online or from any sources about what that might be visiting with pediatrician and some other medical professionals that I'm working with. So curious if you have any thoughts on why reflux happens, what the root causes, and if there's anything else that I can do. Thank you.
So I mean, all babies split up to some extent. So split up is normal, and it is something that parents worry a lot about. But in most cases, it really is just a laundry problem more than anything else. And it is something that typically passes over time as baby's nervous system and neurological system and digestive tract mature. However, sometimes it truly can be more pathological and cause problems with feeding in babies don't want to feed because of it because they experience pain when they feed. And so if a baby isn't truly gaining weight well or is miserable, miserable during feeds, then we really do need to address it. One of my favorite tips for reflux is the breast milk shake. So just helping the fattier part of the milk that the fat you know, sticks to the insides of the milk ducts and helping get that fat in the earlier part of the feed can help the baby to have a little bit more settled tummy after the feeds. bodywork can be really helpful with babies with reflux. If a mother has oversupply the baby's going to be more inclined to have reflux. So we have to look at milk supply issues, you have to rule out tongue tie or palate issues, those can definitely contribute to reflux. And sometimes it's a protein allergy. It's a sensitivity to a protein in the mother's milk from her diet and dairy can sometimes be a culprit in that. So we have to look through all of those things. There's not one simple answer, except she is, the advice that she was given to feed closer together is to me more appropriate than longer apart, because the smaller meals are going to be easier for the baby to digest. And maybe trying to keep the baby in more of an upright position during feeding rather than below the breast. So like football hold can be more difficult for babies who have reflux, and more of like a koala upright position is better.
We have a good real um, you doing a demonstration of the breast milk shake? Yes, we do. People can check that out on our page.
Hey, wonderful humans, I have a question for you all. My name is Kristen, and I'm pregnant with my second baby and planning, another hopeful home birth. And I just had a question around homes and my home in particular. So I know a lot of people say that home is where they feel the safest and the least dressed and all of these things. And in general, I feel that way as well. But we run a business out of our home can be a little chaotic. And sometimes I find the space to not be the most restful or organized, but it's still my home, if that makes sense. And I know I definitely feel safer there than in the hospital. And that's why I've chosen to give to give birth there. But I'm curious if you all have any thoughts around, you know, people like myself, who maybe really want home birth and want that safety and security, but also maybe don't feel the most safe and at ease in their home. But there's not really any other options. And I know this is kind of an odd question, but I just was curious if you'll have any thoughts about that, where if you had any recommendations about ways to make it feel like a little cozier and safer for birth, and just preparing the space in a way that doesn't detract from its daily functionality, because we live in a smaller space, and it gets you. So that's my question. And thank you all so much for everything. Love the podcast, and I've learned so much take care, bye.
You know, toward the end of pregnancy, we really have that natural nesting instinct that kicks in. And I think when that sort of kicks in, you can work your organize your home in a way that makes you feel more ready and prepared to give birth there. It doesn't have to be perfect. It really doesn't. It doesn't have to be the way that she might envision it or see stories on Instagram of people's perfect homes that they give birth. And you don't need that. You just need to feel relaxed enough in your space and not distracted. And I think that nesting instincts is part of why that happens. You know, our bodies aren't expecting to leave the home and go to the hospital. They're expecting to give birth where we are living. That's what our body expects to do. So she might just be unnecessarily worrying about it.
Well, I also think that there's an option to create a very special place wherever she envisions birthing at home because it is a matter of birthing where you feel safest but she did mention that she still would really prefer to birth at home so that's why we're we're we're we're focusing on that not saying well though birth somewhere else. I do think she can set up a beautiful space like the way you set up a little meditation corner in your home. What do you do you keep clutter out of it, you make it look attractive and calming. However you have to do that. You have to get an agreement from everyone else in the house that we're not going to put anything in this space, not mail not clutter of any kind. And just allow yourself to look at that space and envision a beautiful birth there and tell yourself that everything outside of that space doesn't matter.
It doesn't take much it takes maybe some twinkle lights or star lights or something you know soft lighting, some candles, a little music available a tidy space. I do think that tidiness does make people feel feel like they can relax more. Although some people really don't care. I've attended Burson homes that are wildly messy. There, they birth just fine there. Or extremely small. I mean, you can birth in one room. You don't need a huge house. You don't need a completely quiet corridor of your home to give birth.
We've talked on previous episodes about may even making a hospital birth feel more like home and you're right. You don't need to do a lot. A few little things a favorite framed picture to near you and some special lights and your favorite blanket or pillow is really enough. You're working with your mind. You don't need it to be perfect. You're letting your mind attach to something that's calming and then the job is done. That's enough. That's sufficient.
Ladies, my name is Hannah and I have a question about ultrasound accuracy. I was holding my 20 week scan that baby looks completely normal and on track but they did not see a stomach feeling which would suggest that his esophagus is not connected to his stomach, which would be known as esophageal atresia, or tracheal esophageal fistula I already went into the ultrasound very skeptical because I was given a completely false diagnosis of IUGR. With my first one, I'm going to get a second opinion at another hospital in the next few weeks, as I had done with my first time, but just curious in the meantime, if you know anything about esophageal atresia or fistula and the accuracy of this diagnosis in ultrasound, thank you much.
Okay, for this question. Typically, you know, I would give my normal nurse midwifery response, but because we have Liz Idleman coming on the podcast next week, she is going to come on and answer this question today about esophageal atresia.
Hey, Hannah, my name is Liz Eidelman. And I'm happy to chime in here to help answer your question. As I myself am and esophageal atresia mom, my daughter India is now four and a half and thriving. And while esophageal atresia, and tracheal esophageal fistula is often hard to detect on ultrasound, there are some cases, specifically pure EAE without the presence of the fistula that have been detected in utero due to the absence of that stomach bubble. So that said, I would recommend another ultrasound or even a fetal MRI to see if that finding is consistent. There are other anomalies that can be associated with lack of stomach bubble, like facial clefts or diaphragmatic hernias. But seeing as you mentioned, the baby looks otherwise perfect. I'm guessing EA is likely to be the first thing that they'll check for when baby is born. And it's really hard to sit with that uncertainty. But just know that EA is a very treatable outcome. And kids go on to live full typical lives where the people who meet them often have no idea that they even have this diagnosis. So having a tip off in utero is actually a blessing in disguise, because for many ei families, they don't find out until birth, which is myself included. And my own birth story will be airing next week on October 4, it's going to be Episode 233, where I talk about my daughter's diagnosis and her NICU stay. So be sure to tune in for that. And to wrap it up, I would say just use this latter half of pregnancy to set up medical care in a hospital with a strong NICU. And don't forget to celebrate that you are having a beautiful baby. And there might be some challenges, but you will both be okay. And my inbox is always open if you have questions down the road. So wishing you a peaceful pregnancy and a joyful delivery. And thank you as always to Cynthia and Trisha for lending their platform to the EAA community.
All right, thank you, Liz for providing your answer. No doubt, you know much more about esophageal atresia than us put together given your experience and the community that you're in. And in case the name is familiar to anyone out there, Liz Edelman is an influencer with a very, very funny Instagram page, despite the seriousness of her response to Hannah's question, and she's out there, and she made a reference that you can reach out to her so that would be through her Instagram at Liz Eidelman. And again, you'll hear from her directly next week in Episode 233. That is a wrap for this regular episode to hear the extended version of this month's q&a. As always, you can subscribe on Apple, or you can listen as a tier one patron on Patreon. So if you are not in either of those platforms, it is on two quickies.
It is time for quickies. Okay, first one. Why do nurses threatened to put a catheter in you if you don't pee within 20 minutes after giving birth? Oh, because that is so horrible. I can't believe that you that
you should never be threatened with a catheter you should you can be offered a catheter if you are struggling to void after birth. Because if your bladder is really full and you're bleeding and your uterus isn't able to effectively contract because your bladder is full and in the way that you really do want to empty the bladder. And if you're unable to get out of bed for whatever reason, or sometimes the nerves are so overstimulated from pushing that they're not firing and working properly. And so a catheter can actually be helpful. I experienced that my first birth I was unable to be and I was bleeding and I ended up having a catheter at home.
You so you were unable to Why Why were you able
the nerves were so like overstimulated they I couldn't see it. Like the whole normal sensation of ping just wasn't available to me. I couldn't work the muscles and the nerves couldn't work. Oh, that's interesting.
And what is so it can happen is it awful getting a catheter? It sounds it doesn't sound very terrible.
It's not it wasn't terrible.
Oh, wasn't that's good to know.
It's not great, that's for sure. But you know, it's also not great to have a full bladder it feels uncomfortable, which is why it's so important to keep being reminded to get up and go Have the bathroom throughout labor. Go pee go pee, empty your bladder into your bladder. Peppermint oil can be really helpful too. That's something worth trying for a catheter but some not sometimes women I've had women just ask for it. They're like I do not want to get up and go to the bathroom just calf me
really. Okay, what's next? Okay, moving on.
Double nuchal cord and breach at 20 week ultrasound was I was told I couldn't have a vaginal birth. Well, the court has nothing to do with it. The breech? Well, first of all, she's 20 weeks. Breech has means nothing at 20 weeks. So, no, all this is nonsense. If this were an ultrasound at 36 weeks, I would still say the cord means nothing the breech. If you don't have somebody who's willing to support a breech delivery then yeah, C section is you have some decisions to make. Yes, but at 20 weeks, you can't even call it breech at 20 weeks now, you, you you absolutely should not call it breech no 20 weeks, it's technically
the current position of the baby. So you can call it breech because that is the position that the baby is sitting in. So if you have to,
I like to say floating to me breaches more engaged, floating is not on the medical report well, but it should be should be.
All right, best ways to get and keep a baby L O A, which is left occiput anterior. So this is like the optimal position to enter labor. So we've talked about this before, the best thing you can do is keep your center of gravity more forward in late pregnancy. So from 36 to 37 weeks on really trying to avoid being in a reclined position. You can do hands and knees periodically throughout the day, cat cow position, lay on your side, don't spend a lot of time reclined on a couch, sit on a birth ball, keep your belly forward rather than reclined. Right?
And don't stress about it. Yeah,
don't stress about it. The last one, and this is a hard one. So get ready. What, what is the best piece of advice you've ever been given?
Here, everyone listen to yourself on a week? Gosh, that's what we say.
That's so good, though. I thought this was gonna be so hard. No,
I have to think of the best one I was ever given. Let's think one of the, I'm going to share this one because I think it'll be interesting. And I'll give people something to think about. I've always felt my mother is very wise. And when I was a young adult, even, maybe even a teen, she used to talk to me about relationships or finding a partner. And one thing she always said, she said is one of the most important qualities in finding a man. And it's not one that I've ever heard anyone else say. And she said it's generosity. And she said, generosity is a quality that's indicative of so many other qualities. And when someone is generous in one area of their lives, they tend to be generous in all areas of their lives. And, you know, it is one of my favorite qualities in my husband. It's just I just and in many close friends. Megan said, I am extremely positive quality when someone is generous.
That's great. So like that look for generosity and people. They close to those who are generous, I think it says a lot about them.
And when you're saying when we're you're talking about generosity, we're not talking about just material generosity, talking about?
Well, I think material generosity is the indication, usually that they're generous in other areas. I really do not nitpicking not measuring not resenting, not being stingy or withholding. And I think that basically the mindset of not measuring or withholding is just, there's someone who's generous. I just think it's, it's think it's an incredible quality I actually had, I had trouble with my husband when we were dating, because he was so generous, that it started to really concern me about being with him. And I'm, like, we, we had a few times where like, we went to Florida together with another couple we were friends with. And when we went down there, the woman, her godfather lives down there, and she hadn't seen him in a few years. And she told him, she was down in Florida with another couple. And we met the guy and he was like, Oh my gosh, it's so good to see you. I'm going to take all of you out to dinner tonight. And I was like, Oh my gosh, how finally you know this, this, we're going out to dinner this nice place. We were young. And we went out to dinner and the guy was just like he ordered champagne, which I never do it champagne. And that's not common to do at dinner, he ordered champagne. It was like this lavish long dinner. And at the end of it my husband, who was my boyfriend at the time, insisted on picking up the check. Of course, we never saw the man again. And he was like trying to pay and Eric just insisted. And it was because our friend the other guy we were with, used his miles to get us the hotel room for the weekend. And he said well, I just want to give back to them and I'm like, Oh, God, it was like 800. And something dollar was so stressed. Like, this is not going to work. But she liked that. And he did it a few times. I do love that quality in him, I have to say. But he did that we would go out with other couples, and he was constantly insisting on paying if they tried to pay. And I was just like, I don't know how being a financial planner, you know, in that period of my life, I was like, I don't know, I literally don't know how to budget. When I'm with someone who is spontaneously going to spend money like this. If we're saying we're going out to dinner with friends, I I don't think that I'm capable of just saying, Okay, let's budget for a potential $400 dinner now. Like, it really stressed me out. Anyway, so every good quality has its little flip side, right? What about you? Ah,
I don't know. I'm really trying to think on this. Something that comes to mind is once when when I was really bogged down in a difficult situation, in my life, it was kind of all consuming for a period of time a spiritualist told me just very straight up, just be like a giraffe. And I was like, Do you like a giraffe? Does that mean I'm not that tall. And he was like, the higher perspective always look at every situation you're going through in life from the highest perspective, don't be the creature on the ground on the floor, who's like nitpicking over every little detail of life and worrying about how you responded to this or what's going to happen in response to that or like the day to day, just always getting that higher view on life and knowing that everything it from the higher perspective, there's always a larger purpose, a larger path in anything that you experience in life. So when you feel bogged down in the details, when you feel bogged down in the questioning and the analyzing, just really trying to take that step back, have the higher perspective and see all the little players doing their dances and none of it really matters. When you see it from the higher perspective. You just like taking the high road kind of
you know, well it also helps it's kind of like how will I feel about this years from now? It's like oh, years from now, I'm hardly gonna remember the details of this or care about it. Yeah, respective scope, I
know that it's a larger, there's a larger plan involved sort of with everything that you go through. Nice. So it'd be like a giraffe
you like a giraffe. Everyone likes a lot easier from from that place. And don't always pick up the check for everyone. You can't do that we still have to have some kind of balance of practicality in life. All right, well, off we go.
Yes, we gotta go.
Thank you to everyone for submitting your questions.
And don't forget, if you don't want to wait until October to have your q&a question answered. You can always join our Patreon community where you can get your question answered live on the spot, and and off the record private. Yes, those events do not end up in the podcast so you can really ask us anything that is true, either face to face on screen or anonymously. But it is a great space and even if you just joined the first year it is such a great way to support our show. And we give back to you by giving you ad free extended episodes every single month and direct messaging access with us plus some other benefits so we really love to see you over there and we're so grateful to those of you who are already there. And with that said Trisha we actually have a live event happening in 45 minutes so we better prepare for pay for our patrons - I am going to brush my hair.
Thank you for joining us at the Down To Birth Show. You can reach us @downtobirthshow on Instagram or email us at Contact@DownToBirthShow.com. All of Cynthia’s classes and Trisha’s breastfeeding services are offered live online, serving women and couples everywhere. Please remember this information is made available to you for educational and informational purposes only. It is in no way a substitute for medical advice. For our full disclaimer visit downtobirthshow.com/disclaimer. Thanks for tuning in, and as always, hear everyone and listen to yourself.
Recent Episodes
Subscribe
Between episodes, connect with us on Instagram @DownToBirthShow to see behind-the-scenes production clips and join the conversation by responding to our questions and polls related to pregnancy, childbirth and early motherhood.
You can reach us at Contact@DownToBirthShow.com or call (802) 438-3696 (802-GET-DOWN).
To join our monthly newsletter, text “downtobirth” to 22828.
We'd love to hear your story.
Please fill out the form if you are interested in being on the show.
Subscribe to The Show
Follow Us On Social