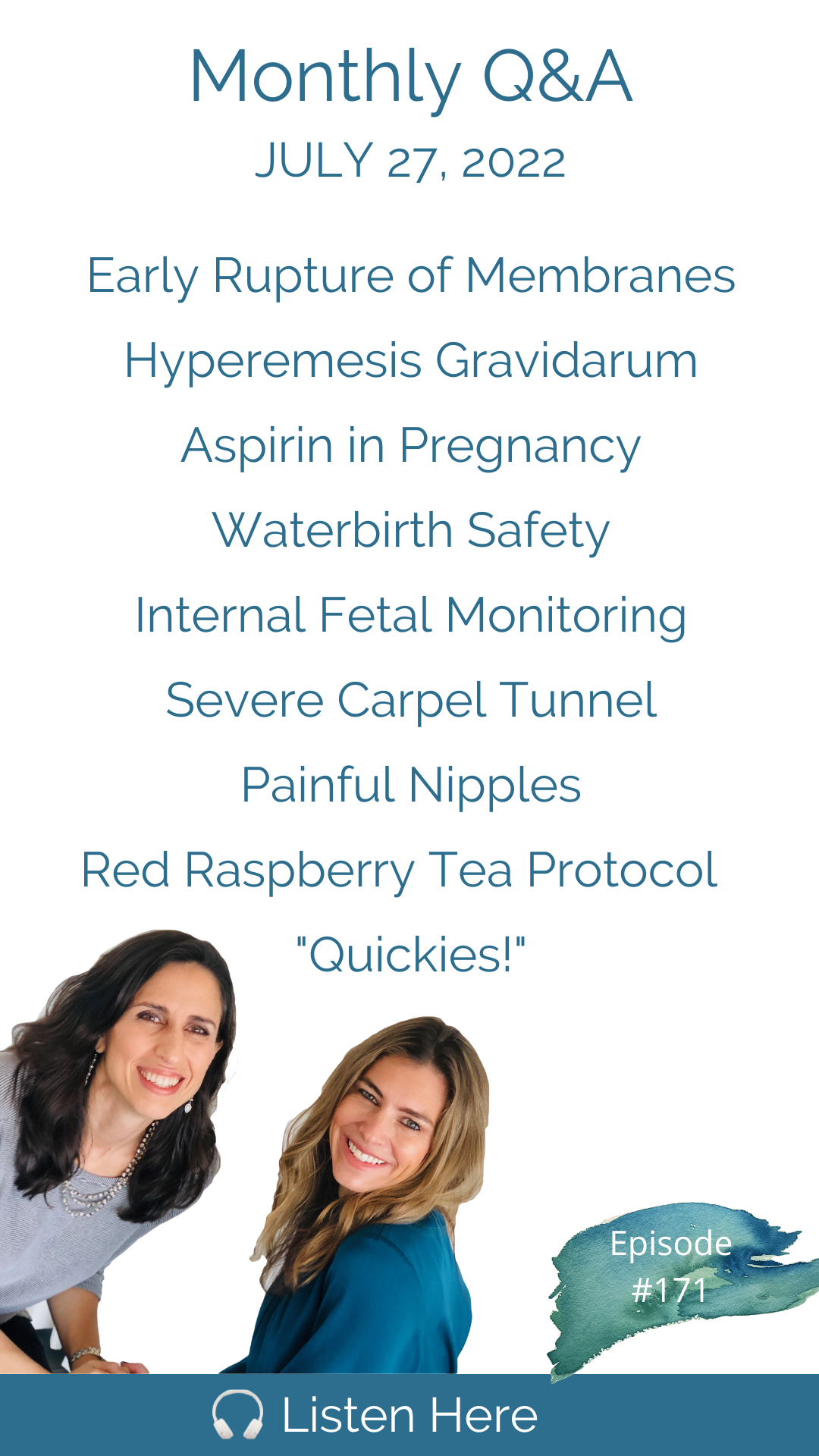
It's the last Wednesday of the month, and you know what that means! We are back with our monthly Q&A episode. Today, we are discussing how long it is safe to go after your bag of waters releases (see link to our amazing birth story below); What can be done to treat or prevent Hyperemesis Gravidarum? Is Aspirin in pregnancy really necessary and what does ACOG have to say about it? When your hospital says waterbirth increases the risk of infection and is harmful to the baby--is that true? The world-expert in water birthing, Barbara Harper, founder of Waterbirth International, steps in to answer this one. And one woman was told her uterus wouldn't be "safe" to have another baby for one year. Also, is it normal to have nipple pain in pregnancy and how will this impact breastfeeding...and quickies! Remember you can access the extended, ad-free version of this episode by subscribing on Apple. This month's extended version includes: Severe carpel tunnel in pregnancy and what can be done about it; Fetal scalp electrode monitoring: what is it, and do the benefits ever outweigh the risks? You'll hear our thoughts on this "extreme" intervention; Having a two-vessel umbilical cord that was identified during the 20-week anatomy scan; What's the lowdown on red raspberry leaf tea? What are the benefits, and when/how much to consume during pregnancy. Thank you as always for your excellent questions and see you next week! If you would like to submit a question, please call and leave us a message with your question at (802) 438-3696 That's 802-GET-DOWN. (Cute, right?) #78 | Christina's Run From Induction to a Home Birth with Group B Strep ********** This show is sponsored by: Connect with Cynthia and Trisha at: Work with Cynthia: Work with Trisha at: We serve women and couples coast to coast with our live, online monthly HypnoBirthing classes, support groups and prenatal/postpartum workshops. We are so grateful for your reviews and shares! Please remember we don’t provide medical advice, and to speak with your licensed medical provider related to all your healthcare matters. Thanks so much for joining in the conversation, and see you next week!
Silverette USA*
DYPER*
NOM Maternity*
Vyana Infant Massage*
Wildbird.co*
Beautiful Births and Beyond*
Postpartum Soothe*
*Use promo code DOWNTOBIRTH
Hi, Cynthia and Trisha is your biggest fan girl here with a question. Recently, a friend of mine was told that she should wait one year postpartum before trying to conceive again so that her uterus is safe. I am calling you from Seattle. My question is about baby aspirin and pregnancy. I was wondering if you know or have heard of anyone ever successfully preventing hyperemesis gravidarum in pregnancy? My question is, do midwives ever use fetal scalp electrode monitoring? And when did the risks outweigh the benefits? Ever since basically, the start of my pregnancy, I have had some incredible nipple pain. So much. So that's a big old flag.
That's like a negative point. If you get points for having a tub, that's a negative point, you have a tub and you use it for storage. That's just definitely worse than not having a tub.
I'm Cynthia Overgard, owner of HypnoBirthing of Connecticut, childbirth advocate and postpartum support specialist. And I'm Trisha Ludwig, certified nurse midwife and international board certified lactation consultant. And this is the Down To Birth Podcast. Childbirth is something we're made to do. But how do we have our safest and most satisfying experience in today's medical culture? Let's dispel the myths and get down to birth.
Hello, everyone. Welcome to the July q&a. Why don't you tell everyone the exciting new format we have this month.
This is gonna be really fun. You guys called in and left voicemail questions on our phone number and we are going to do our q&a this month with your recorded questions.
It's so different hearing voices is that it's so nice. Yes. Just the way you guys you know the little subtleties in in tones and they all sound like great people we want to hang out with. It's really fun this way. They sound like they sound like our friends. And you know what, just in all in all truthfulness? Trisha, we were never that good at reading questions. We never really nailed that skill. We had. We had a lot of outtakes where we were fumbling over question. Oh,
thank you. Are we had to restate? Or, of course, anyway. Yeah. Because yeah, sometimes the way you read it, write a question and read a question. It just doesn't always line up.
Yeah, it's hard to read conversational things. I think that then like reading a book. Yeah, this is interesting. This new format though, guys are we hopefully will, will be smooth with it. But it's our first time. So bear with us.
Now. It's gonna go great. It's gonna go great. I'm really excited to get started. So let's jump in with the first question. We have tons of questions, we just want to remind everyone, if you would like much longer q&a, many more questions. Remember to subscribe on Apple. And all of our episodes, including back in season one and two, every single episode, I believe, is entirely ad free. So exclusive content longer q&a every single month, and no ads ever. So if that isn't enticing, I don't know what it is. But it's all out there. So we are very excited to see the subscribers we have. And thank you so much. And we want to reward you certainly with really great content. And Trisha that means we have a ton of questions to record today. So some of which for the for the regular episode and some pretty extensive let's jump in. Alright, let's go. Here's our Here's our first question.
I've been doing Trisha, my name is Pearson. And I've been listening for a couple years now from down here in Central Texas. I love this podcast so much. I actually had a hard time thinking of a question because you'll have just taught me so much. But I just think of one related to my first birth. So I had pre labor rupture of membranes the day after my due date, just a little leak. And I went in to see the hospital based midwives that I was going to after letting them know what happened. The midwife actually said that she wanted me to be in active labor 24 hours past my water breaking, and she was actually encouraging me to come in right away for induction. I am so glad that I heard her but listen to myself and my intuition. And I opted to go home and just let labor start naturally. I went on to give birth to my son later that evening with no issues but I'm still so uncomfortable with the idea that had my labor not started as quickly as it did. I would have been pressured or coerced into induction. That 24 hour clock just felt so arbitrary and the situation then a lot of red flags that for me. So my question would be at what point is there a real indication for an induction after PRM or pre labor rupture of memory Once again, thank you both so much for all the wisdom and environment.
So I would open this discussion by saying that there is no reason to induce unless you have a medical indication. And while many obese and some midwives may say that preterm rupture of membranes is a medical indication, I think you and I would both agree that it is not should you develop a fever, that's different story. But she also mentioned that she had a small leak.
Well, preterm also would be like if the baby would be premature, that would be an issue. Yes, she didn't. She didn't think you did. I think you just said preterm ruptured membranes.
I did. I may have said preterm what I meant premature. So there is also such thing as preterm premature, this is just premature rupture of membranes at term, she said she has a small leak, which means that she may have just ruptured a four bag of waters and that really does not provide a lot of opportunity for infection to ascend into the uterus. A Frank rupture in combination with anything in the vagina such as a cervical exam can put you at increased risk of infection or increased risk of developing a fever. Her midwife wanted her to come in right away and said, Ah, that she expects that she will be in labor by 24 hours. And that's because most women 90% of women who frankly rupture their bag of water will go into labor by 24 hours, labor will have begun by them. That's an important distinction from having the baby born by then. So women have to understand like to be your your, you're agreeing wholeheartedly with that, right? Because 100% Yeah, yeah, because sometimes women think, oh, gosh, like I only, you know, 22 hours in and nothing's happened. But I think it is worth talking about this, because labor begins for only 10 or 15% of women with their membranes releasing and no other sign of labor. And historically, everyone gets excited that the baby is coming. And you find yourself casually walking out to the car, let's say to go to the hospital or the birthing center, you put on your seatbelt, and you're driving there with your partner, like Oh, labor really isn't so bad. It's pretty like it's, this is fine. And the thing is, you're done in labor, and the hospital will be happy to take you. And before you know it, you're in the room, you're in the bed, they're going to start telling you you're having some kind of failure to something or other they're going to start pushing drugs. And right there, it's increasing those adverse outcomes, those unnecessary cenarion sections. So this is a really good question that's being asked what it is arbitrary that this is 24 hours, some doctors are so aggressive as to say we want to see you here within 12 hours if your group B strep negative, you want to jump in?
Yeah, I was gonna say I don't think 24 hours is arbitrary. I think it's based on the fact that 90% of women will go into labor by 24 hours. So the assumption is that if you don't, there's something abnormal, but there but there really isn't. And even HR is starting to soften their language around it. Their guidelines as of a couple of years ago, we're getting really soft around saying it's women have been observed up to a few days with no change in the outcomes. ACOG is saying that now. Right. And they're also depends on as I said earlier, it depends on if it's a frank rupture or a small leak. It's not the same thing to your right. Right, right. But what I was saying earlier, if your group B strep negative, if you're at full term, there really is no concern. And if you do have one of those really high intervention, doctors who says, well, we need to see you in here. Listen for rhetoric, listen for, you know, we get concerned we don't want to we don't want to see you. What we don't want is for you to have your membranes releasing over 24 hours. That sounds really scary when you listen to it. But if you really break it down, that's just rhetoric. So you can say what's the risk of Group B strep, negative? Now, if you group B strep, positive, that is a different story. But if you're negative what what are they worried about? What infection are they talking about?
It's really infection. I mean, you don't have to have Group B strep to develop a fever.
But however, yeah, but I mean, bacteria doesn't travel up through the vagina and even if that's the concern, you can ask for a prophylactic antibiotic. So I guess the point is, call your provider. Drink. First of all, drink water and keep drinking water if your membranes release call your provider if your GBS negative, remind them of that. And by time read those ACOG guidelines because they certainly should follow those at a minimum and there again, they're getting very soft around they're getting a lot softer around that allowing more time and you should take your you should take your temperature because just having a fever is does put the baby at risk. But you shouldn't develop a fever if nothing goes in the vagina. So keep things out of the vagina. Keep a Cynthia set hydrating because your amniotic fluid for the baby will continue to replenish even if your water is broken. It's not that it's not that your baby is gonna have no amniotic fluid. It does continue to keep on replenishing, and that fluid is a great resource for your baby that helps with fetal positioning along the way. So you want to think in terms of the baby having that resource.
If you want to listen to a really inspiring story, Cynthia you I'm gonna count on you to remember the episode about the birth story. And I'm not even gonna remember it was way back in the beginning. The mother who Christina who had five days of Christina Yeah, February of 2021. Christina fire chippers with my mentor Nancy Waner. Yeah, five days of ruptured membranes that might be that might be my favorite birth story that we've had so far. I it's hard to pick a favorite but that that is definitely one of the few that I always recommend to all of my clients. I think that's a Yeah, I can't pick a favorite. Now the other ones I love are coming to mind. But that that one is worth a listen. That one is a very, very worthwhile episode for sure. I loved her perspective and her everything about it. We got a ton of questions. We gotta move along here. Okay, let's go.
Hi, Cynthia. And Trisha, I was wondering if you know, or I've heard of anyone ever successfully preventing hyperemesis gravidarum and pregnancy, I was diagnosed with both of my pregnancies, and a husband and I both want more kids, but I am literally terrified of being pregnant again. Thanks.
Hyperemesis gravidarum is extreme nausea and vomiting of pregnancy.
Well, it can be debilitating. So nausea and vomiting of pregnancy is a thing for most people. But it's of course, a scale. And if it becomes if it becomes so severe that you can't keep down food and water, and it's impacting your ability to gain weight and sufficiently eat in pregnancy, then it becomes HGW. And it can be very serious, because if you aren't able to keep down food and water, you're obviously not going to be able to give enough hydration to your body, you can get dehydrated, you can get completely depleted nutritionally, it can impact your baby's growth. So we do have to pay attention to it and and remedy it, it is very much a spectrum. Should it be severe enough that you do you become dehydrated you you do need to go for IV therapy. I think it's also really helpful to identify triggers, knowing the foods that do make you feel nauseous. So do I know of how to completely prevent it the next time around? No, I don't I mean, some women will have a subsequent pregnancy and not have it most if they had it in their first pregnancy, I would say probably more than half, maybe even 75% Experience it a second time. But you can do some things to try to reduce it. So that would be things like really learning to identify the foods that are triggers for you even expanding the foods that you eat, like when you're not pregnant, widening your variety of interest in foods so that new foods and pregnancy might be easier for you. Certain smells in the house can be triggers. So if you have fragrances that you knew bothered you the last time make sure those things are completely out of the house whether that's like laundry detergents, soaps, candles, getting in really good physical shape can help so it is more common in women who are slightly even just slightly to moderately overweight, that is a risk factor. So being in good physical shape can make a difference. Whatever that means for you know for you we all know when we're sort of like in our best shape versus not thought about a specific BMI or anything like that.
You haven't named the thing that helps my friend Suzanne Okay, so oh you're about to say acupressure, your best wristbands, the C bands is that what she used now? Okay, well acupuncture, acupuncture and acupressure. accute acupuncture and acupressure are both helpful for reducing nausea and vomiting of pregnancy.
Okay, my friend Suzanne. First of all, all three pregnancies, severe severe, just like she she's from Minneapolis, her mother in law from Texas had to fly and stay with her because she couldn't take care of her children and my friend is extremely fit. She was an athlete in most, you know, most of her life. She She's one of the most joyful and maybe the most joyful person that I know she's like always in this incredibly delightful mood and it was it was incredible to see her go through this because I would call her and she was lying in bed all the time. She couldn't function happened to all three pregnancies. I'm so sorry to say that because the woman writing in is afraid to get pregnant again. But It Suzanne's I think it was her mother, or third pregnancy who said, I made you an acupuncture appointment. And it was like month six or seven, she went and immediately vanished. It all went away, it all got better with acupuncture. I'm not the least bit surprised, because I feel like I could tell a dozen stories of acupuncture, turning things around for people. So please take heart, if you want to have another baby. Don't be too discouraged. Because hopefully all these things will work. But definitely keep acupuncture as a part of your life, maybe even pre conception, I would, I would say 100% preconception. Really trying to get your body in the best nutritional state is really important as well like eating what very nutrient dense food taking a good prenatal vitamins start getting all your vitamin and mineral stores in a good place so that if you are not able to keep food down as much, you're your body's not going to get depleted as quickly. Also, filtering water is important because there could be certain things in the water that are aggravating and making you feel nauseous. And then just basic stuff that we recommend for nausea, nausea and vomiting of pregnancy in general, like eating small, more frequent meals, not drinking on an empty stomach when you wake up in the morning. Oh, if it's really severe like it is for this woman joining a support group. And those exists because this is really hard for women and it's making it so she doesn't want to get pregnant. So having that extra support makes a huge difference.
Okay, so for this next one, we received two questions asking different variations of the same question related to a recommendation from a provider to take baby aspirin in pregnancy. So first, let's hear both of those questions that were submitted. And then we'll respond.
Hi, Cynthia and Trisha, I am calling me from Seattle. Love your show. My mom actually told me about it and I started listening, learn so much. And so I just want to thank you for that. My question is about baby aspirin and pregnancy. I was told by the CNM at the hospital based practice that I was going to that I should start taking low dose aspirin starting after 12 weeks I think was 12 or 13 weeks they recommended that I start daily on a low dose aspirin to help reduce the risk of preeclampsia and not against it. But I'm really curious what your take is the reasons that they gave me were the risk factors were first pregnancy and over a 35 at the time of delivery, and I'll be 36. Exactly. I'm 35 now, and I'll be 36 at delivery. So I'm curious what your take is on this. I would love more information that just wasn't quite enough for me. So anyway, thank you so much love your show and appreciate all that you ladies do. Hi, Cynthia. And Trisha, my name is Kate, I'm calling from Massachusetts. I'm calling with a question of Brown, baby aspirin and preeclampsia. I saw a nurse practitioner today here in the Boston area for an appointment. I am in my early 40s. And I was asking her about being a first time pregnant, possibly being a first time pregnant mom in my early 40s. And she mentioned that the practice where I had the appointment has a policy about starting all pregnant patients over the age of 40 on baby aspirin at 12 weeks to prevent preeclampsia. So my questions are around this because this has to be standard practice over the age of 40. Does it help to do this? And alternatively, could it be determined through testing and other evaluations that this regime might only make sense for some pregnant people and not for everyone? She did not answer my questions when I inquired further. So maybe you can both shed some light on this because I would just love to know more. And maybe there are others out there who will be interested to know too wonderful to have this opportunity to reach out. Have a lovely day. And thank you for all that you do. I'm following you both on Instagram, enjoying all of the content and listening to your invaluable, insightful podcast to keep up the amazing work and it's so greatly appreciated. Take care, but aspirin in pregnancy. This is an area I really care about for no particular reason other than I've noticed in working with couples since 2007. That about I don't know 789 years ago, I started hearing women I'm working with sharing with me that their providers are telling them to take an aspirin a day now. Does it really make sense to take an aspirin every day in the name of health? It never felt right to me. So let's look at the research on this. This is a recent trend that medical caregivers are recommending low dose aspirin in pregnancy. According to ACOG, the American College of Obstetricians and Gynecologists This is a quote low dose aspirin prophylaxis should be considered for women with more than one of several moderate risk factors for preeclampsia. This is very important, more than one moderate, not low risk, moderate risk factors for preeclampsia. ACOG goes on to say that a relative risk reduction is probably just two to 5%, two to 5%. They're having women go on daily aspirin when it really provides a possible relative risk reduction of just two to 5%. Aspirin is not recommended for women with unexplained loss, or as a routine preeclampsia preventative there we go that exactly addresses the question we received today. But again, I want to say women with unexplained loss, so about half of losses are unexplained. This would not make sense for them or routinely to prevent preeclampsia, regardless of your age. However, that's exactly the trend we're seeing. We're seeing that it's being recommended routinely. To prevent preeclampsia, or simply because of age, we are even seeing low risk first time women over 35 of being advised to take a daily aspirin in pregnancy. So if they say like you're an older mom that puts you at higher risk of preeclampsia or stillbirth. Don't take any chances just take a low dose aspirin every day. That's classic rhetoric and ACOG expressly disagrees with it. According to ACOG also, and this is a quote in the absence of high risk factors for preeclampsia. The current evidence does not support the use of prophylactic low dose aspirin for the prevention of early pregnancy loss, fetal growth, restriction, stillbirth or preterm birth. ACOG says low dose aspirin is considered safe, and it is associated with a low likelihood of serious maternal or fetal complications. So that's interesting because it's a qualitative comment bordering on rhetoric, low risk of serious maternal complications indicates that there Are are some potential serious complications. That's how we have to read between the lines with these things. According to the Mayo Clinic, higher doses of aspirin pose various risks various risks in pregnancy during the first trimester potential pregnancy loss, and congenital defects. Again, this is with a high risk. I mean, this is with a high dose. And during semester in the first trimester, and during the third trimester increased risk of premature closure of a vessel in the fetuses heart, and also increased risk of bleeding in the brain of premature infant infants. It's important to note the Mayo Clinic only named risks associated with high doses as we just said, but if high doses can cause severely adverse health effects, should we really be routinely giving low doses to so many women with a relative risk reduction of just two to 5%? Trisha?
That's pretty small number. I think the point the take home is that it's being routinely offered for women that ACOG clearly states, it's not recommended for and it's certainly not recommended, because you're over age 40, which is also what we hear with no risk factors for any other reason other than being 40.
Yeah, you have to have several moderate risk factors. Several they don't even say one, right. That's pretty was a very thorough review of that. Of that topic. Thank you.
I got all that a few times about that. Oh, yeah. Sorry that it was such a rant on that. But no, it's good. When you do the research, you've got to keep reading. Like if they say, well, then who? You know, you want to say like, Well, where are there gaps and miss? Who is it good for? So there you go.
95% of you, it is not going to be good for you, at least.
Hi, Cynthia. Hi, Trisha. I hope you guys are doing well. My name is Sabrina. I'm from New Brunswick, Canada. And I was actually calling regarding a question. So I recently went to see my OB, and she asked them if we could do a water birth. They explained that they do have a tub, but they choose not to use it. And then she also said that it might be broken, but they're also just using it as a storage room. But they choose not to practice waterbirth because there is a increase in infection. And as well as more difficulties with regulating the baby's temperature. I don't believe that to be true. Um, I've been listening to your podcast for almost my entire pregnancy. And I really wanted to say thank you for all the information you put out there. Because of everything I've learned from your podcasts, I've actually chosen to switch practitioners last week, and I'm currently 36 weeks pregnant. So I'm getting some better care now, in my opinion, but hope to hear what you guys have to say on that and have a great day.
Trisha, I have a surprise for you.
Yeah. I mean, I just it's so nice when we get such a straightforward, easy question like this where there's no oh, well, if this scenario, you might need to do this. It's like this is just No, no wrong and wrong. Everything about this is wrong.
And well, I just love like well that we have one tub, but it's broken. And we use it for storage. We use it for storage, it's filled with crap right now. I mean, what kind of places that it's like, well, we made that effort, but you know, no one used it. They would say that, like they like to say that we have we have a tub. We have it it's you know, it's on their website. We offer waterbirth or labor in the tub or whatever. But Trisha, I have a surprise for you. I reached out to Barbara Harper, who we both love, of course, and she's been on the podcast twice. She is the world expert hands down in water berthing. She's the founder of waterbirth International, which she founded in the 80s. And I shared this audio recording with her and she called back and gave us an audio recording in response. So we have amazing we have her response right here.
Hi, this is Barbara Harper reporting from Denver, Colorado. And I'm here to answer Sabrina's questions about infection and keeping baby warm. Sabrina, I would if you could not go to that hospital. And if you must, then bring your own tub in. The research is overwhelming for understanding that there are no increases in infection for either mother or baby. Even the Cochrane Database, and the UK says no adverse outcomes for either mother or baby. As early as 1960 There was a study published in the OBGYN A journal in the US that said bath water does not enter the vagina. So as far as keeping the baby warm, the in a waterproof every baby goes to mother's chest, I call it the sanctuary, and your chest has thermo receptors that measure the baby's temperature every four seconds sends that information to your brain, and your chest warms up. Now, when I attend a water birth, we put the baby in the sanctuary of the mother's chest. And then I'll put, after a few minutes, I'll put a warm towel behind baby. I've never had a baby that was difficult to regulate their temperature. And we keep mothers and babies skin to skin. Good luck with your birth. And if you need more information, send a message to barbara@waterbirth.org and visit waterbirth.org as well as waterbirth i n t and v Barbara Harper. Take care. God bless.
That was very nice of her.
And now everyone can get a sample of what a wealth of knowledge is. Every four seconds thermo receptors in your chest are assessing your baby's temperature and sending that information to your brain. I mean, it's just mind blowing. I know that with when women have twins, if one has a fever, that one breast will cool accordingly. So I guess that's how it all happens behind the scenes. But please do look up our episodes with Barbara episode 100. The benefits the benefits of water birthing, and 122 provider green lights. That was a pretty remarkable conversation with her in her work traveling the world educating doctors and nurses in how to support water birthing.
And please don't have your baby at any hospital if at all possible that uses their tub as a storage room.
Right? That's a hard read that's like a firm red flag.
That's a big old flag.
That's like a negative point. If you get points for having a tub that's a negative point. You have a tub and you use it for storage. That's just definitely worse than not having a tub.
Yes it is.
Hey ladies, my name is Katie. I'm from Belleville Kentucky area. I've been listening to your podcast now for roughly 12 weeks. I'm 35 years old and have waited eight years to become pregnant and finally have had a successful IVF procedure. So now I'm currently 23 weeks pregnant. I do have a question. I am fully hoping to breastfeed that's my plan y'all to help plans go. But ever since basically the start of my pregnancy I have had some incredible nipple pain. So much so that even just grazing like an article clothing and T shirt after the shower you know counting down it just hurts so bad. So I have become very anxious now about the possibility of breastfeeding. So I was just curious if this ever goes away. If there's anything I can do to alleviate the pain Yet again, thank you guys so much. I love love, love the podcast out on Instagram. I'm totally addicted. Thanks again guys. How nice.
That was very nice, I would try to help her feel a little more relaxed about postpartum that her nipples may not feel the same way after the baby is born as they do right now in pregnancy, sometimes people do get really really sensitive nipples in pregnancy. It's just one of the changes that happens with pregnancy and it does not mean that that's going to be intensified during breastfeeding. If the baby is latching, well, there really shouldn't be any nipple pain associated with breastfeeding. If her nipples are bothering her right now in pregnancy, she can even start to use some of the things that we recommend during breastfeeding like smoothies or even silver at something to keep the nipple from rubbing on her bra or on fabrics or on a towel. If it's related to spasm. Sometimes if the nipples get cold or wind or something, you know expose the nipples get exposed to something they contract as they're meant to. And that can create a lot of pain for women if they're especially sensitive. Where if they have basal spasm and the nipple, so putting some pressure on it can help. But the overall thing would be just that she's that's does not mean that her nipple pain is going to be more intense after the baby's born.
High Cynthia and Trisha is your biggest fan girl here with a question. Recently, a friend of mine was told that she should wait one year postpartum before trying to conceive again so that her uterus is safe. Now after listening to your podcasts, I've become very skeptical when medical providers mentioned the word safe. Is there any truth to this? And can you speak to this? Love your podcast and I wish I knew about it when I was pregnant. Thank you so much.
So I'm not I'm not sure why your uterus is unsafe after a vaginal birth. Right? I mean, I think it's good for your body to give it 12 months or so between pregnancies just to give your body time to replenish its nutrient and mineral stores. It's good for your mental health to wait a little bit longer in between babies. And it's just good for your overall physicality, your physical body to have time to recover, we lose a lot of strength in our core in pregnancy. And, you know, we can get depleted nutritionally, we can get depleted in lots of ways after having a baby so I think 12 months is a good idea from all those perspectives, but it has nothing to do with your uterus being safe or not.
Yeah, I resent that language a little bit. Who's to call someone else's body part unsafe? Like how would any woman want to feel that there's an organ in her body that isn't safe? I don't I don't think it's a good choice of words. Anyway, that just sounds like rhetoric. I know you know it, Sarah, but you can now tell her we agree with you on that point. Time for quickies.
Hey, Cynthia. And Trisha. This is Kate. I was wondering if you guys have any tips or tricks to get comfortable while in the third trimester when you feel like you just can't be great. Thanks.
Get in the bath.
Get in the bath. That's your answer to everything. That's always your answer to everything
is the answer to all ailments. All right. Epsom salt tub.
All right. Epsom salt tub. Next quickie.
Hi, my name is Kristen. And I'm calling from North Carolina. I started listening to your podcast when I found out I was pregnant. And I heard on the episode The other day you talking about brain? The acronym and I can't remember what it stands for. Could you refresh us? Thanks.
Well, this is such a good one. All right, brain. Let's see if I can remember. What are the benefits? What are the risks? What are my alternatives? What does my intuition tell me? And what happens if I do nothing? So the brain acronym is something that you can use anytime you are faced with a difficult decision. Or you have a question for your provider that you do not feel as being answered properly, then or thoroughly enough, go through the brain acronym in your head and ask your provider those all of those things, benefits, risks, alternatives, intuition, doing nothing and love the last two in particular, I mean, they're all great, but intuition is the one that no one really thinks about and doing nothing is a really important alternative that usually gets overlooked. What if we do nothing? Or what if we wait, exactly. Next?
Hi, Trisha. And Cynthia. I'm so grateful for your show. I am wondering if you would touch on which supplements and brands do you recommend for pregnancy, breastfeeding and postpartum? There is just so much information out there about like, take this versus that. And it's kind of overwhelming. I eat a pretty healthy whole foods diet, and I'm wondering what I really need and what I should prioritize. Thank you.
That is not a quickie. Yeah, that's not a quickie. But let's give some quick info. A quick response I can give is, if you have insurance, and your doctor prescribes one, that is probably the one of the worst things on the market, because it's all kemri. NATO, you're talking? Yeah. prenatals Yeah, yeah. Prescriptive prenatal. Yes. Yeah, those are the words. They're the worst quality, the most expensive ones. So of course, your doctors are inclined to to partner up with their buddies and pharma which they are buddies. I did an Instagram thing this week about how they share a lobby with them. But those are the worst things for you. So whatever you do, you can go to like a whole foods, but look for something that's food based. That's the first thing. No corn, no soy, no gluten, no animal, like just pure pure. But my mentor would say, put much more of your energy into what's on your plate, what you're actually putting in your body. And she likes to think of prenatals as optional because she wants women to feel so good about how they're eating that they don't have to supplement. But of course, supplementing is perfectly fine and good. When you have a good quality. You want to add any quick comments on that topic? Yeah, really quick, I would just say that I would buy my prenatal vitamins from a good reputable supplement company. So not just something that you find at CVS or target but like something from a vital nutrients or Thorne is a good company or pure encapsulations is a good company and get your pre medical just get your prenatal with methylated folate because you never know if you're somebody who needs that more, more than others. And it usually is a better quality prenatal vitamin in general, and for postpartum, postpartum Su, of course, postpartum sube. Yeah, she said, postpartum what to take for postpartum? Yeah, but that's topical. But can she just ask about herbs? Oh, okay, cool. Yeah, I was pregnant soon. All right, last one.
Hi, Trisha. And, Cynthia, This is Leanne from Washington State. And I am curious about why it seems to be the standard of care. Well, at least for the midwives in my area to do chord attraction. I mean, I understand the importance of that stage of labor. But it feels a little counterintuitive. I would love to hear your thoughts on that. Thanks so much go by. But as the midwife say it Well, I think it's it's standard of care, because it's an old part of the act of management of third stage of labor. And again, this would not really be a quickie, but it shouldn't be standard chord direction does not need to be routine, it should not be standard. But it probably comes from that place where they just haven't dropped it yet. For the active management of labor of the third stage of labor is the use of Pitocin. And cord traction, to deliver the placenta and describe cord traction. Cord traction just means putting extra pressure on the vocal, pulling tugging on the cord to help birth the placenta.
Yep, I'm not a fan of that. It can increase the likelihood of pulling out the placenta prematurely and having retained placenta, and also just again, overkill, can we just leave everyone alone, please, like this woman just gave birth? We have to be tugging on the organ that's attached on the inside of her body? Because we're in such a hurry to get it out? I don't think so. So I, you know, I think this woman's intuition is right. And, and her midwives really shouldn't be doing that. And she has the right to say not to do that to her. Right. I mean, no, no one should handle you without your consent. So if that's what they do, that's what they can do to somebody else if they allow it, but you don't have to allow it. There's no need for it. I mean, there has to be a good reason for it. What would be one good reason for it.
I mean, if the mother is actively hemorrhaging, you know, you might use some contraction to get vitamins out.
Okay. Yeah. All right, everyone. Before we sign off, just remember to submit any question to our monthly q&a is call us at 802-438-3696. That's 802 Get down. And you can leave us a message there at any point. 24/7 That was fun. That was so great. Everybody's voices put down to birth show in your contacts, and we'll just be a phone call away. I wonder if the people who subscribe now are like it's too many questions. It's too much.
I doubt it. All right.
Well, I'm gonna see you. You have a lactation consultant appointment right now. And you're meeting me.
Should I just meet you right at the restaurant at fancy dinner not looking fancy. So you're passing through you're gonna do that again. Sorry I gotta walk out the door in 30 seconds I don't get time to change oh man All right I'll dress down dress down, baby.
Thank you for joining us at the Down To Birth Show. You can reach us @downtobirthshow on Instagram or email us at Contact@DownToBirthShow.com. All of Cynthia’s classes and Trisha’s breastfeeding services are offered live online, serving women and couples everywhere. Please remember this information is made available to you for educational and informational purposes only. It is in no way a substitute for medical advice. For our full disclaimer visit downtobirthshow.com/disclaimer. Thanks for tuning in, and as always, hear everyone and listen to yourself.
I shall never forget inserting a fetal scalp electrode as practicing the student midwife.
Oh no.
It was very unpleasant experience for you or for her for me and her and the baby or me.
I'm sure it was for two. Yeah, and it will also was for me
because you didn't want to be doing it. Yeah, just felt cruel to just screw that into the baby's head.
Is that the only time you ever did it?
I mean a few times in your training midwifery school I did it but not in practice. Never in practice. No, not at home birth. We don't even have that.
Recent Episodes
Subscribe
Between episodes, connect with us on Instagram @DownToBirthShow to see behind-the-scenes production clips and join the conversation by responding to our questions and polls related to pregnancy, childbirth and early motherhood.
You can reach us at Contact@DownToBirthShow.com or call (802) 438-3696 (802-GET-DOWN).
To join our monthly newsletter, text “downtobirth” to 22828.
We'd love to hear your story.
Please fill out the form if you are interested in being on the show.
Subscribe to The Show
Follow Us On Social